Abstract
Objectives
The traditional, subject-based medical teaching mode has gradually transitioned to a system-based integration mode. This study aims to provide the experience of design and implementation of a pilot program to integrate a “cardiovascular system” curriculum into an eight-year medical education in Xi’an Jiaotong University in China.
Methods
We launched a curriculum integration project that includes study of the cardiovascular system in the eight-year medical education course. Curriculum integration was carefully designed. An integrated curriculum team was formed and the integration objectives clearly defined. The content to be integrated was identified and various tasks were assigned. The perceptions of students and teachers were evaluated using a questionnaire survey.
Results
We first integrated pharmacology into the new curriculum. This progressed from physiology through pathology to pathophysiology, and finally, to the principal therapeutic drugs. The “cardiovascular system” curriculum was divided into six functional parts: morphological structure; cardiac electrophysiology and relevant drugs; coronary circulation and relevant drugs; cardiovascular function, diseases, and relevant drugs; heart failure and therapeutic drugs; and other cardiovascular diseases.
Conclusions
An integrated curriculum centered on organ systems has been successfully established using the cardiovascular system as a pilot. Both students and teachers perceived that all cardiovascular system blocks were well-integrated.
Introduction
Harvard Medical School, one of the best medical colleges in the world, radically reformed the medical curriculum in 1985. The “new pathway” of medical education contains nine novel, integrated curriculum modules that effectively incorporate basic and clinical medicine [1]. The aim is to solve clinical problems. This approach has greatly influenced medical teaching worldwide. In the past decade, the School of Medicine at the University of California, Los Angeles (UCLA), has gradually reformed the original curriculum system. National Yang-Ming University built a complete and functional integrated curriculum over the course of 10 years. Compared to American students, those trained in National Yang-Ming University exhibited similar pass rates on the United States Medical Licensing Examination. Given such success, the traditional subject-based teaching mode has gradually transitioned to a system-based integration mode [2].
Commencing in 2004, the Chinese government directed several colleges and universities to strengthen science and engineering education. To this end, the initial five-year course of education gradually turned into an eight-year course in most medical colleges and universities [3]. The ultimate goal of medical education is to cultivate excellent qualified clinicians. An eight-year medical education program is by no means a simple “5 + 3.” Of note, the 2022 National Education Conference in Beijing stressed the importance of improving the quality of education, accelerating its modernization, building a strong system, and preparing students to become well-rounded individuals. These are to be morally integral, intellectually knowledgeable, physically healthy, esthetically sensible, hard-working, and industrious people. The conference established new requirements and higher goals for medical education. It was imperative to pursue educational reform. However, most medical colleges and universities in China still engage in spoon-fed medical education. This does not encourage systematic thinking or independent learning.
Xi’an Jiaotong University, one of the oldest universities in China, is a key university that is under the direct administration of the Ministry of Education of China. This is a comprehensive research university that focuses on 10 major disciplines, including medical education. In total, 4496 undergraduate students are enrolled in medicine-related majors including the eight-year program of clinical medicine, stomatology, pharmacy, basic medicine, nursing, and other majors. Our medical school still generally uses the traditional subject-based teaching mode. Based on the demand for educational reform, our school selected study of the cardiovascular system as a pilot program when integrating the curriculum of eight-year medical education. Our school has established cooperative and exchange relationships with the National Yang-Ming University of Taiwan, China, and the UCLA School of Medicine [4], 5]. These efforts are supported by the Kwang-Hua Education Foundation (Taiwan, China). Drawing on their successful experience [6], we engaged in preliminary exploration and practice, and then launched our problem-based learning (PBL)-driven curriculum integration project in China.
Methods
After preliminary theoretical evaluation and field testing, an integrated curriculum centered on the cardiovascular system was successfully established (Figure 1).
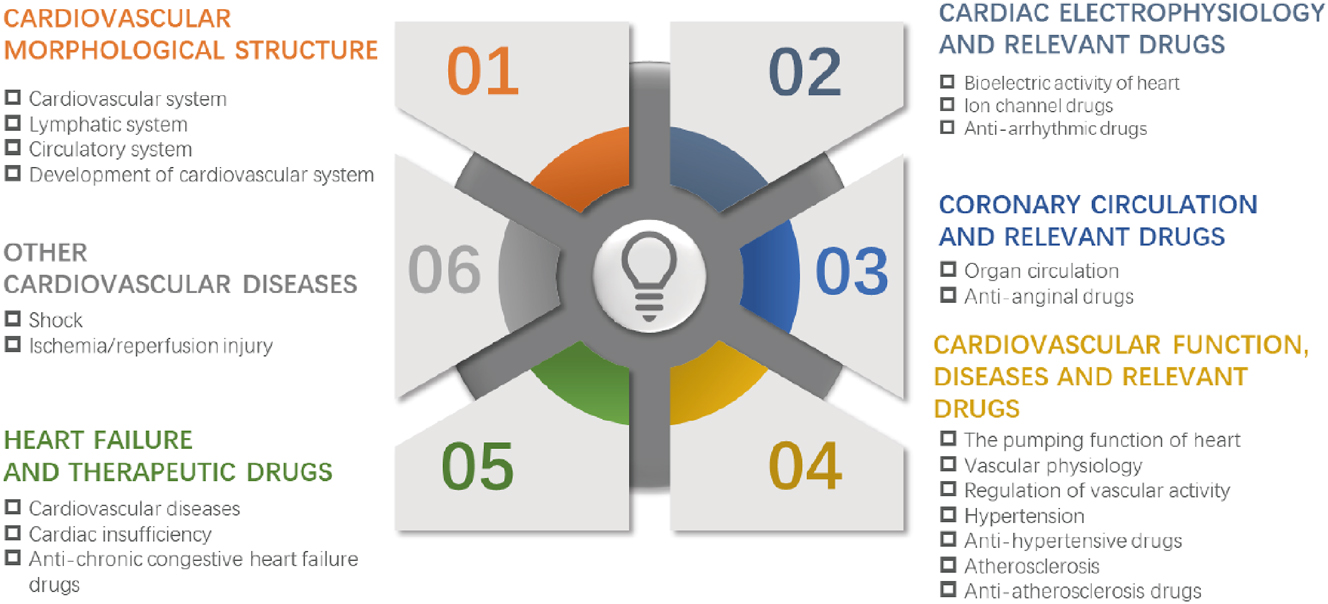
Diagram of an integrated curriculum centered on the cardiovascular system. The “cardiovascular system” curriculum was divided into six functional parts, including cardiovascular morphological structure, cardiac electrophysiology and relevant drugs, coronary circulation and relevant drugs, cardiovascular function, diseases, and relevant drugs, heart failure and therapeutic drugs, and other cardiovascular diseases.
Curriculum integration design
Studying the cardiovascular system involves human anatomy, histology, embryology, pathology, physiology, pathophysiology, pharmacology, and other disciplines. We integrated the cardiovascular curriculum with consideration of the characteristics of human cardiovascular diseases and the cognitive abilities of students. After integration, the “cardiovascular system” curriculum became sequentially organized in terms of morphology, structure, function, disease, and pharmacology. We systematically expounded the anatomical cardiovascular structure, the embryogenesis, morphological and functional characteristics, diseases, and drugs targeting the cardiovascular system. The integrated course accounts for 80 % of the marks, and PBL 20 %. The two parts are mutually complementary. Materials not covered in the integrated course are learned via PBL.
Building of an integrated curriculum team
An Organ System Integration Curriculum Office was established to coordinate the work among experts in various disciplines and to implement teaching operations. Students in the eight-year medical program take integrated courses during their third, fourth, and fifth years. In total, 35 medical courses were reduced to 12 courses that integrated organ systems. The cardiovascular system is one such system. We are currently integrating courses on 11 other organ systems, including introduction to human biology, musculoskeletal system, sensory and nervous systems, endocrine system, host defense system, blood and oncology, respiratory system, digestive system, urinary system, reproductive system, and growth and development. We will establish a complete organ system-based curriculum. In total, 181 students in the eight-year medical education system took part in the reform. It is essential that teachers understand the purpose and the plan of curriculum integration. This ensures high quality and a successful outcome. Teachers who wish to participate in the integrated curriculum voluntarily sign up and get well-trained. The experts discuss matters among themselves and choose the most competent teachers. The teaching team is composed of one experienced cardiologist, along with other teachers based in the departments of anatomy, embryology, pathology, physiology, pathophysiology, and pharmacology. After the basic framework of the system was determined, a series of teacher seminars were organized. It was sought to constantly improve the curriculum via exchanges and discussion, and to promote teacher thinking on the integrated curriculum. Under the overall planning of the director of the “Cardiovascular Curriculum Integration Project” in our school, these teachers mutually cooperate to ensure that the content of their courses is fully integrated with that of others.
Clarity of integration objectives, determination of the content to be integrated, and assignment of tasks
After careful investigation, practical demonstrations, and frequent meeting discussions, the director of the “Cardiovascular Curriculum Integration Project” defined that the objective of the integrated “cardiovascular system” curriculum constitutes part of the eight-year medical education program in our school. Then, the selected teachers mentioned above discussed what elements of their disciplines required integration, and how to do that. Of note, the teachers decided unanimously that knowledge of marginal and interdisciplinary content, and of frontier scientific discoveries, should be enhanced in the new curriculum. For example, polygenic genetic diseases are discussed in the cardiovascular module. These aid in the understanding of the pathogeneses of hypertension and atherosclerosis.
Connections between PBL and basic theory
Functional and structural heart diseases were studied via PBL. The “cardiovascular system” curriculum thus includes two PBL cases with eight or nine students in each PBL group. Two tutors (a clinician and a basic medicine teacher) facilitate a PBL session. First, the clinicians choose two vivid, representative, and comprehensive cases that further the learning objectives. These cases are sent to experts for review, followed by modification and processing based on the experts’ opinions. In class, such content is omitted, being reserved for the PBL sessions. Organ system-based assessment is integrated. The views of students and teachers who completed the integrated course on the “cardiovascular system” were sought via a questionnaire survey. The maximum score for each item was 4 on a Likert scale, where 1 was strongly disagree, 2 was disagree, 3 was agree and 4 was strongly agree. The data were analyzed using GraphPad Prism software and are expressed as mean ± SD.
Results
Integration of basic theory
In cooperation and communication with the UCLA School of Medicine and National Yang-Ming University, we established a new method whereby theoretical courses could be integrated based on the characteristics of our university. We first added pharmacology to the “cardiovascular system” curriculum. This progresses from physiology through pathology to pathophysiology, and finally to the key topic, appropriate therapeutic drugs. Students are exposed to the complete courses of cardiovascular diseases. After many discussions and practical trials, we integrated the cardiovascular contents of related disciplines, but this was by no means only a simple addition. Rather, we reintegrated the topics by their respective characteristics and formed functional modules that exhibited cognitive regularity. Our integration was strictly logical. This renders the content more coherent, greatly reduces teaching hours, eliminates repetition, and includes the latest frontier knowledge. What we presented to students was thus a relatively independent, but interrelated and graded, theoretical system. The “cardiovascular system” curriculum was divided into six functional parts. The relevant disciplinary features and the required class hours are shown in Table 1. Such in-depth integration significantly reduced the class hours from 64 to 42 h, thus to 65.6 % of the former figure. This gave students more time to study independently and established a good foundation for the combination of theoretical courses and PBL teaching. After the teaching content was integrated, redundant disciplinary knowledge was reduced. This enhanced student understanding and clinical application of basic knowledge. Students had stronger medical/clinical thinking and improved ability of problem solving and independent learning [7].
Functional modules and class hours of the “cardiovascular system” curriculum.
| Functional module | Discipline | Chapter | Content | Class hour (after integration)/h | Class hour (before integration)/h |
|---|---|---|---|---|---|
| Cardiovascular | Systematic anatomy | 1 | Cardiovascular system | 3 | 7 |
| morphological structure | Systematic anatomy | 2 | Lymphatic system | 1 | 1 |
| Histology | 3 | Circulatory system | 2 | 2 | |
| Embryology | 4 | Development of cardiovascular | 2 | 2 | |
| system | |||||
| Cardiac electrophysiology | Physiology | 5 | Bioelectric activity of heart | 2 | 4 |
| and relevant drugs | Pharmacology | 6 | Ion channel drugs | 1 | 1 |
| Pharmacology | 7 | Anti-arrhythmic drugs | 2 | 3 | |
| Coronary circulation | Physiology | 8 | Organ circulation | 1 | 1 |
| and relevant drugs | Pharmacology | 9 | Anti-anginal drugs | 1 | 1.5 |
| Cardiovascular function, | Physiology | 10 | The pumping function of heart | 2 | 4 |
| diseases, and relevant drugs | Physiology | 11 | Vascular physiology | 2 | 3 |
| Physiology | 12 | Regulation of vascular activity | 3 | 4 | |
| Pathology and pathophysiology | 13 | Hypertension | 2 | 2 | |
| Pharmacology | 14 | Anti-hypertensive drugs | 2 | 2 | |
| Pathology and pathophysiology | 15 | Atherosclerosis | 2 | 2 | |
| Pharmacology | 16 | Anti-atherosclerosis drugs | 1 | 1.5 | |
| Heart failure and | Pathology | 17 | Cardiovascular diseases | 4 | 8 |
| therapeutic drugs | Physiopathology | 18 | Cardiac insufficiency | 3 | 4 |
| Pharmacology | 19 | Anti-chronic congestive heart | 2 | 3 | |
| failure drugs | |||||
| Other cardiovascular | Physiopathology | 20 | Shock | 2 | 4 |
| diseases | Physiopathology | 21 | Ischemia/reperfusion injury | 2 | 4 |
| Total | 42 | 64 |
Cardiovascular morphological structure
The cardiovascular morphological structure module is taught principally by anatomy and embryology teachers. Students gain a comprehensive understanding of the morphology, structure, and development of the cardiovascular system.
Cardiac electrophysiology and relevant drugs
The morphological structure of the heart is the basis of its electrical activity. If the structure of the heart is mastered, further study of the electrical activity yields twice the result for half the effort. Students then find it easy to understand how ion channels and anti-arrhythmic drugs target the electrical activity. In the traditional model, these three components were studied in the freshman, sophomore, and senior years, respectively. Students often forgot the prior knowledge and thus found it difficult to connect the components.
Coronary circulation and relevant drugs
The coronary artery circulation delivers energy for the entire heart. Arterial blockade induces ischemia and angina pectoris. Some students have encountered angina patients and may thus be eager to know the optimal treatment. However, in the old teaching mode, pharmacology and physiology were taught in two different semesters, seriously compromising learning continuity and the lively nature of a good teaching form.
Cardiovascular function, diseases, and relevant drugs
The first three modules deal with the pumping function of the heart and regulation of vascular activity. Students thus acquire a clear and complete understanding of the cardiovascular system, which helps them to better understand and master the pathogeneses of hypertension and atherosclerosis, and the actions of anti-hypertensive and anti-atherosclerosis drugs, thereby ensuring the consistency of knowledge.
Heart failure and therapeutic drugs
The endpoints of cardiovascular diseases such as hypertension and atherosclerosis are heart failure, which can be treated using certain drugs. Study of these topics in a logical manner, thus in interlocking sequence, maintains students’ interest.
Other cardiovascular diseases
Shock and ischemia/reperfusion injury are classified into other cardiovascular diseases.
Integration of experimental studies
Integration of the “cardiovascular system” curriculum does not lower practical standards. Experimental teaching is indispensable during medical education. When integrating the experimental classes, we removed duplicate experiments and divided the new and retained experiments into two modules, morphological and functional, completed in dedicated morphological and functional centers, respectively. The details are shown in Table 2.
Experimental class hours of the “cardiovascular system” curriculum.
| Functional module | Discipline | Experiment content | Class hour (after integration)/h | Class hour (before integration)/h |
|---|---|---|---|---|
| Morphological experiments | Systematic anatomy | Cardiac anatomy and physiology | 4 | 4 |
| Systematic anatomy | Arteries anatomy | 4 | 4 | |
| Systematic anatomy | Veins and lymphatic vessels anatomy | 4 | 4 | |
| Histology | Observation of vascular tissue | 2 | 4 | |
| Pathology | Observation on specimen and tissue section of cardiovascular system | 4 | 4 | |
| Functional experiments | Physiology | Blood pressure measurement, heart sounds auscultation and electrocardiogram examination | 2 | 0 |
| Physiology and pharmacology | Regulation of cardiovascular activity and effects of efferent nervous system drugs on blood pressure | 4 | 4 | |
| Pathophysiology and pharmacology | Arrhythmia and the effect of anti-arrhythmic drugs | 4 | 4 | |
| Pathophysiology and pharmacology | Establishment and experimental treatment of acute heart failure animal model | 4 | 4 | |
| Total | 32 | 32 |
Effectiveness of curriculum integration
A questionnaire was used to evaluate curriculum integration in terms of the cardiovascular system. The overall mean student score was good (3.5 ± 0.5), as was the overall mean teacher score (3.4 ± 0.5) (Table 3). The mean teacher perception of logical sequencing of different disciplines within each integrated block was good (3.5 ± 0.5). The student score was (3.2 ± 0.4). This suggests that deeper insight into the knowledge system for students may be required. Both students and teachers perceived that the new “cardiovascular system” curriculum integrated not only basic science but also clinical science and societal aspects (Table 3).
Questionnaire survey to students and teachers.
| Items | Description | Perception of students (n=181) | Perception of teachers (n=65) |
|---|---|---|---|
| Item 1 | Organization of different disciplines within each integrated block is logical | 3.2 ± 0.4 | 3.5 ± 0.5 |
| Item 2 | Relevant topics are covered in same week, which renders the content more coherent | 3.3 ± 0.5 | 3.4 ± 0.5 |
| Item 3 | The content of different disciplines in each integrated block is closely connected | 3.4 ± 0.5 | 3.5 ± 0.5 |
| Item 4 | The new “cardiovascular system” curriculum integrates basic science with clinical science | 3.5 ± 0.5 | 3.5 ± 0.5 |
| Item 5 | The new “cardiovascular system” curriculum integrates basic science with societal aspects | 3.2 ± 0.4 | 3.3 ± 0.5 |
| Item 6 | Early clinical exposure is provided in the integrated “cardiovascular system” curriculum | 3.6 ± 0.5 | 3.7 ± 0.5 |
| Item 7 | Experimental studies are aligned with the integrated “cardiovascular system” curriculum | 3.4 ± 0.5 | 3.5 ± 0.5 |
| Item 8 | The integrated “cardiovascular system” curriculum is aligned with PBL cases | 3.6 ± 0.5 | 3.6 ± 0.5 |
| Item 9 | PBL is a major learning methodology that integrates the various basic science disciplines in the “cardiovascular system” curriculum | 3.5 ± 0.5 | 3.6 ± 0.5 |
| Item 10 | Integrated curriculum fosters student learning and improves knowledge retention | 3.6 ± 0.5 | 3.7 ± 0.4 |
| Overall score (mean ± SD) | 3.4 ± 0.5 | 3.5 ± 0.5 |
-
Scoring criteria: 1, Strongly disagree; 2, Disagree; 3, Agree; 4, Strongly agree. PBL, project-based learning; SD, standard deviation.
Discussion
Given the developments in human healthcare and the changes in the spectrum of human diseases, modern medicine has evolved from a simple biomedical model to a biological–psychological–social discipline. When treating patients, it is necessary to understand the biological causes of the disease, the pathophysiological mechanisms in play, and the possible prognoses and outcomes. However, it is also important to understand the social and mental states of patients and to tailor treatment to their social circumstances and family environments. The “global minimum essential requirements” of the Institute for International Medical Education include clinical skills, population health, professional values, attitudes, scientific foundations, critical thinking, communication skills, and information management [8]. All doctors must acquire these competencies. Today, medical education features new requirements and higher goals than before. It is imperative to further foster educational reform.
Developments in medical science have been associated with the emergence of many interdisciplinary, intradisciplinary, and comprehensive fields of study. The old disciplinary boundaries are no longer clear. The traditional teaching mode is no longer adequate. There is an apparent general trend that disciplinary barriers are broken because knowledge is becoming fused. About half of the 178 winners of the Nobel Prize in Physiology or Medicine from 1901 to 2002 were from the United States. Most experts and scholars believe that the key to such success lies in the solid form of pre-medical education. Most students acquire a bachelor’s degree in science or engineering before entering medical school. In recent years, when building a brand-new model of medical education, medical schools in the United States successfully reformed the traditional education model of subject-based teaching. Today, teaching features system-based integration combined with PBL. Students learn by working in groups to solve an open-ended problem. The problem thus drives learning. Globally, medical education is being innovatively improved to include team-based learning (TBL), PBL, and case-based learning (CBL). To these, the recent case-based collaborative learning (CBCL) introduced by Harvard University should be added [9]. All feature organ-system-based integrated curricula.
It is thus clear that reform of the eight-year Chinese medical education program is urgent. Pilot studies aid the direction of program development. The “curriculum integration + PBL” model has become popular in many medical colleges and universities worldwide and more recently, in certain Chinese medical colleges and universities. The Peking University Health Science Center has been exploring curriculum integration for some time. By breaking the increasingly artificial boundaries between related disciplines such as basic and clinical medicine, medical knowledge acquisition is being reorganized with a focus on the various organ systems. Reform in Xi’an Jiaotong University commenced with the introduction of an integrated study of the cardiovascular system. This forms part of the eight-year study program. The aim is to produce doctors and physicians of high quality. Our school has established cooperation and exchange relationships with National Yang-Ming University of Taiwan, China and the UCLA School of Medicine. Drawing on their experience, we launched our PBL-driven curriculum integration project. We successfully integrated the “cardiovascular system” curriculum that is part of the eight-year medical education program. The class hours fell significantly from 64 to 42 h. The organ-system-based, integrated curriculum reduces knowledge redundancy, creating more opportunities for competency-oriented medical education and independent learning. Both students and teachers reported that the integrated “cardiovascular system” curriculum was successful. Real-world medical practice is interdisciplinary. The curriculum improved clinical thinking and allowed students to use comprehensive knowledge of the cardiovascular system when solving problems. The curriculum fostered student learning, improved knowledge retention, and cultivated a holistic clinical mindset.
Based on the success of the “cardiovascular system” curriculum, we plan to integrate all courses on other organ systems. We will build a fully organ-system-based curriculum similar to those of our peers worldwide. We seek to contribute to the development of medical education and ensure excellent physician training. The Chinese government has implemented the Healthy China 2023 Project that provides policy support for teaching reform. Only by “breaking through and then standing up” can we make great progress. Higher medical education in China must prosper with the goal of training excellent clinicians.
Funding source: Training Program for Top Students in Basic Medicine 2.0 Teaching Reform Research Project
Award Identifier / Grant number: 2205
Award Identifier / Grant number: 2202
Funding source: Shaanxi Higher Education Teaching Reform Research Project
Award Identifier / Grant number: 21BY005
Funding source: Natural Science Foundation of Shaanxi Province
Award Identifier / Grant number: 2024JC-YBMS-612
-
Research ethics: Not applicable.
-
Author contributions: Zheng Wang worked on the analysis and interpretation of data, drafting the article. Xinglong Zheng worked on acquisition of data and analysis and interpretation of data, revising the article. Dongmin Li, Liesu Meng, Yuan Wang, Xi He, and Jinjun Liu worked on the Integration of Cardiovascular Curriculum for Eight-year Medical Education Program, revising the article critically for important intellectual contents. The authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Informed consent: Not applicable.
-
Conflict of interest: The authors state no conflict of interest.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Research funding: This work was supported by Shaanxi Higher Education Teaching Reform Research Project [grant number 21BY005] and Training Program for Top Students in Basic Medicine 2.0 Teaching Reform Research Project [grant numbers 2205 and 2202] and Natural Science Foundation of Shaanxi Province [grant number 2024JCYBMS-612]
-
Data availability: All data supporting the reported results were showed in figures and tables included in the present manuscript.
References
1. Dienstag, JL. Evolution of the new pathway curriculum at Harvard Medical School: the new integrated curriculum. Perspect Biol Med 2011;54:36–54. https://doi.org/10.1353/pbm.2011.0003.Search in Google Scholar PubMed
2. Anderson, DM. Overarching goals, values, and assumptions of integrated curriculum design. SCHOLE A J Leis Stud Recreat Educ 2013;28:1–10. https://doi.org/10.1080/1937156x.2013.11949690.Search in Google Scholar
3. Wu, H, Xie, A, Wang, W. Eight-year medical education program: retrospect and prospect of the high-level medical talent training in China. ECNU Rev Educ 2021;4:190–209. https://doi.org/10.1177/2096531120957665.Search in Google Scholar
4. Chang, CC, Lirng, JF, Wang, PN, Wang, SJ, Chen, CH, Yang, LY, et al.. A pilot study of integrating standardized patients in problem-based learning tutorial in Taiwan. J Chin Med Assoc 2019;82:464–8. https://doi.org/10.1097/jcma.0000000000000109.Search in Google Scholar
5. Fan, APC, Kosik, RO, Tsai, TCC, Cai, Q, Xu, GT, Guo, L, et al.. A snapshot of the status of problem-based learning (PBL) in Chinese medical schools. Med Teach 2014;36:615–20. https://doi.org/10.3109/0142159x.2014.902045.Search in Google Scholar
6. Brauer, DG, Ferguson, KJ. The integrated curriculum in medical education: AMEE Guide No. 96. Med Teach 2015;37:312–22. https://doi.org/10.3109/0142159x.2014.970998.Search in Google Scholar
7. Shrivastava, SR, Shrivastava, PS. Scope of organ system-based curriculum in the delivery of medical education: a critique. Indian J Health Sci Biomed Res 2020;13:262. https://doi.org/10.4103/kleuhsj.kleuhsj_117_20.Search in Google Scholar
8. Core Committee, Institute for International Medical Education. Global minimum essential requirements in medical education. Med Teach 2002;24:130–5. https://doi.org/10.1080/01421590220120731.Search in Google Scholar PubMed
9. Schwartzstein, RM, Dienstag, JL, King, RW, Chang, BS, Flanagan, JG, Besche, HC, et al.. The Harvard Medical School pathways curriculum: reimagining developmentally appropriate medical education for contemporary learners. Acad Med 2020;95:1687–95. https://doi.org/10.1097/acm.0000000000003270.Search in Google Scholar PubMed
© 2025 the author(s), published by De Gruyter on behalf of the Shanghai Jiao Tong University and the Shanghai Jiao Tong University School of Medicine
This work is licensed under the Creative Commons Attribution 4.0 International License.


