Abstract
Objectives
Intracranial hemorrhages are common events in premature infants but in fetal life those incidents are often of ominous prognosis and unknown etiology.
Case presentation
We present the diagnosis, evolution and management of a fetal hemorrhagic accident associated with an inherited maternal microdeletion of the chromosome 16 short arm. Abnormal neurosonography in routine second trimester ultrasound led to follow up. Fetal germinal matrix hemorrhage along with severe asymmetric ventriculomegaly and a secondary periventricular cyst developed in the early third trimester. Array CGH showed microdeletion 16p11.2.
Conclusions
This microdeletion had not been previously associated with fetal intracranial hemorrhage.
Introduction
Ischemic or hemorrhagic accidents in utero are extremely rare events of ominous prognosis and no effective treatment known that can lead to neurodevelopmental impairment [1]. These accidents are most commonly diagnosed in the newborn. Besides, fetal stroke is associated with prematurity, metabolic disease, intertwin transfusion syndrome, infectious or drug exposure, trauma or coagulation disorders. In absence of these causes a genetic etiology can be suspected [2]. In a recent meta-analysis the authors found several genes related to idiopathic antenatal intracranial hemorrhage: pro-inflammatory cytokines, collagen genes and X linked GATA1 gene mutation [2]. On the other hand, fetal microdeletions usually manifest in utero as malformations and are suspected upon the finding of ultrasound anomalies or soft markers.
Microdeletion 16p11.2 has been related to developmental delay, intellectual disability, and/or autism spectrum disorder, obesity, and an increased frequency of congenital defects with IQ being even in the normal range [3]. The deletion, which was first reported in individuals with autism spectrum disorder and learning disabilities, has been related to a variety of neuroimaging findings such as posterior fossa malformation and periventricular heterotopia [4] but has not previously found associated with fetal intracranial hemorrhage.
We present the diagnosis, evolution and management of a fetal hemorrhagic accident associated with a maternal inherited microdeletion of the chromosome 16 short arm.
Case presentation
We present the case of a 39 year-old healthy patient with a history of infertility and no consanguinity. The patient was overweight (BMI 28.9) and this was her second pregnancy after a previous miscarriage. This pregnancy was achieved by embryo transfer after two failed in vitro fertilizations.
The first trimester aneuploidy screening ultrasound at week 12 + 3 was normal with CRL 55.6 mm and nuchal translucency 1.6 mm (59 centile). The results of the first trimester combined screening were: MoM PaPP-A 1.42, MoM HCG-Beta 1.46, trisomy 21 risk 1/1544.
Routine ultrasound scan at 22 week gestation showed small cavum septum pellucidum (2.3 mm; −2 SD for gestational age) (Figure 1), as well as parallel anterior frontal ventricular horns. Hypoplasia of corpus callosum was suspected and reevaluation took place in a week. At 22 weeks gestation corpus callosum was 15 mm and posterior ventricular horns measurement was 8 mm. Once informed, the couple opted for invasive testing and molecular karyotype.
Transverse view of the fetal head at 22 weeks gestation showing small cavum septum pellucidum.
At 26 weeks fetal growth was within normal percentiles, corpus callosum was normal and posterior ventricular horns measured 12.8 mm. Array could not be assessed due to contamination but conventional karyotype was normal. New array and maternal serologic TORCH analyses were offered and performed.
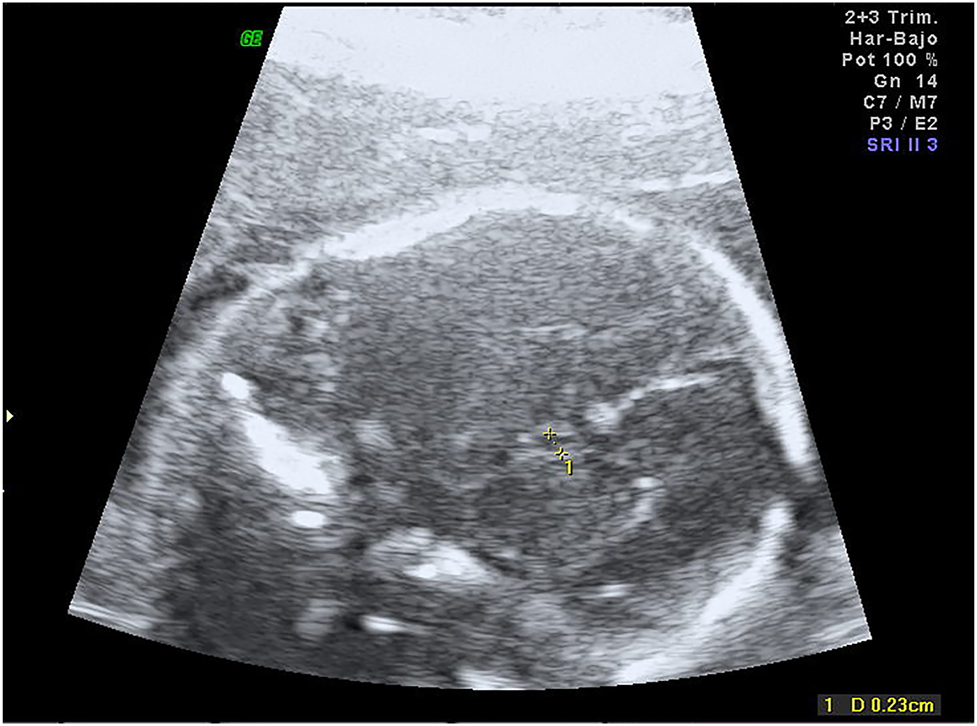
At 30–32 weeks fetal growth remained normal and asymmetric ventriculomegaly developed, the right ventricle posterior horn reached 14 mm and there were signs of germinal matrix hemorrhage along with a secondary periventricular cyst (Figure 2, Supplemental Material, Videos 1 and 2). There was periventricular echogenicity and a complicated periventricular cyst. Medium cerebral artery Doppler showed no signs of anemia. Thrombophilia, infectious diseases screening (toxoplasmosis, parvovirus, cytomegalovirus, listeria), and antiplatelet antibodies studies were negative. CGH Array demonstrated a microdeletion in the short arm of chromosome 16, 16p11.2 (28682192_29076269)x1.

Transvaginal ultrasound at week 32 showing asymmetric ventriculomegaly and periventricular cyst.
Magnetic resonance imaging at week 32 showed severe dilatation of the left cerebral ventricle up to 20 mm and altered subcortical sign in the left hemisphere suggestive of ischemical, toxic vs. infectious insult (Figures 3 and 4).

Fetal MRI at week 32 showing severe ventriculomegaly.

Fetal MRI at week 32 showing axial view of asymmetric ventriculomegaly.
Parents underwent counseling by a multidisciplinary team including ann a neurology pediatrician and a geneticist. The patient opted for pregnancy termination and refused necropsy. Fetal specimen showed normal phenotype. Severe postpartum hemorrhage occurred due to uterine atony and resolved after medical treatment and uterine tamponade.
Carrier status study was offered to the couple and the mother was found to be a carrier of the same deletion. This copy number variant implies a 50% risk of recurrence.
The patient opted for embryo donation and two years later gave birth to a healthy newborn after an uneventful pregnancy which ended in labor induction for prolonged pregnancy. Severe postpartum hemorrhage recurred again in absence of placental abnormalities and was controlled with conservative management.
Discussion
Fetal cerebral hemorrhagic insult has not been previously associated with 16p11.2 microdeletion to the best of our knowledge. We could not find other causes for the fetal intracranial hemorrhage or the patient’s recurrent postpartum hemorrhage.
Fetal hemorrhage developed in the late second trimester and was diagnosed upon follow up of suspected hypoplastic corpus callosum. Cavum septum pellucidum can be seen between weeks 18–37 in the normal fetus; non visualization has been described in a variety of cerebral anomalies, especially in cases of corpus callosum hypoplasia or agenesis [5]. Normal ranges have been described by Falco et al. [5]: in week 21 cavum should measure between 3.4 and 6.2 mm. In the present case it was below −2 ds The diagnosis of short corpus callosum can be a false positive if made at an early gestational age, therefore, measurement should be repeated at least 4 weeks after the routine second trimester ultrasound.
In the present case, the 390 m kb microdeletion is associated with neurodevelopmental anomalies with a penetrance of 62.4% [6]. The deletion of the 16p11.2 region is linked to variable phenotype including obesity, behavioral disturbances and craniofacial dysmorphism [7], all of which our patient did not show. Ventriculomegaly and periventricular nodular heterotopia with seizures has been described in children affected with this deletion [4]. Chung et al. recently published a review on the medical, behavioral and neurological characteristics of deletion or duplication carriers [7]. They concluded that the deletion is most often de novo, but is inherited in approximately 7% of probands; it is related to autism, motor coordination difficulties, seizures, obesity, etc. and there is significant phenotypic variability among carriers. Bijlsma [8] reported on an adult who had a small deletion (200 kb) and worked as a truck driver and had learning difficulties as a child, he passed the microdeletion on to his son, who had a learning disability. Our patient works as technician in a research laboratory and has normal phenotype and no history of other bleeding disorder.
Prenatal diagnosis of the presence of this microdeletion has only been reported once in a case of fetal diaphragmatic hernia [9]. Gelfand et al. [10] studied 13 cases of perinatal arterial ischemic stroke and found that apolipoprotein E polymorphism may confer genetic susceptibility for perinatal arterial ischemic stroke. This gene is located in chromosome 19. Other authors have not found any genetic underlying condition in a series of fetal intracranial hemorrhage [11].
We hypothesize that the microdeletion was responsible for an structural abnormality that led to hemorrhage, although the lack of necropsy impairs a definite etiologic diagnosis.
We can conclude that after the diagnosis of suspected fetal intracranial hemorrhage a diagnostic workup is recommended and should include CGH array with the possibility of extending to exome.
Acknowledgments
Dr. de Luis and Dr. Flores for their assistance.
-
Research funding: None declared.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Competing interests: Authors state no conflict of interest.
-
Informed consent: Not applicable.
-
Ethical approval: The local Institutional Review Board deemed the study exempt from informed consent.
References
1. Dunbar, MJ, Woodward, K, Leijser, LM, Kirton, A. Antenatal diagnosis of fetal intraventricular hemorrhage: systematic review and meta-analysis. Dev Med Child Neurol 2021;63:144–55. https://doi.org/10.1111/dmcn.14713.Search in Google Scholar PubMed
2. Cavaliere, AF, Turrini, I, Pallottini, M, Vidiri, A, Marchi, L, Perelli, F, et al.. Genetic profiling of idiopathic antenatal intracranial haemorrhage: what we know? Genes (Basel) 2021;12:573–82. https://doi.org/10.3390/genes12040573.Search in Google Scholar PubMed PubMed Central
3. Miller, DT, Chung, W, Nasir, R, Shen, Y, Steinman, KJ, Wu, BL, et al.. 16p11.2 recurrent microdeletion. In: Adam, MP, Ardinger, HH, Pagon, RA, Wallace, SE, Bean, LJH, Mirzaa, G, editors, et al.. Gene Reviews((R)). Seattle, WA: University of Washington; 1993.Search in Google Scholar
4. Miller, D. 16p11.2 microdeletions. Available from: https://www.rarechromo.org/media/information/Chromosome%2016/16p11.2%20microdeletions%20FTNW.pdf. 2019 [Accessed 2 Jul 2021].Search in Google Scholar
5. Falco, P, Gabrielli, S, Visentin, A, Perolo, A, Pilu, G, Bovicelli, L. Transabdominal sonography of the cavum septum pellucidum in normal fetuses in the second and third trimesters of pregnancy. Ultrasound Obstet Gynecol 2000;16:549–53. https://doi.org/10.1046/j.1469-0705.2000.00244.x.Search in Google Scholar PubMed
6. Rosenfeld, JA, Coe, BP, Eichler, EE, Cuckle, H, Shaffer, LG. Estimates of penetrance for recurrent pathogenic copy-number variations. Genet Med 2013;15:478–81. https://doi.org/10.1038/gim.2012.164.Search in Google Scholar PubMed PubMed Central
7. Chung, WK, Roberts, TP, Sherr, EH, Snyder, LG, Spiro, JE. 16p11.2 deletion syndrome. Curr Opin Genet Dev 2021;68:49–56. https://doi.org/10.1016/j.gde.2021.01.011.Search in Google Scholar PubMed
8. Bijlsma, EK, Gijsbers, AC, Schuurs-Hoeijmakers, JH, van Haeringen, A, Fransen van de Putte, DE, Anderlid, BM, et al.. Extending the phenotype of recurrent rearrangements of 16p11.2: deletions in mentally retarded patients without autism and in normal individuals. Eur J Med Genet 2009;52:77–87. https://doi.org/10.1016/j.ejmg.2009.03.006.Search in Google Scholar PubMed
9. Genesio, R, Maruotti, GM, Saccone, G, Mormile, A, Conti, A, Cicatiello, R, et al.. Prenatally diagnosed distal 16p11.2 microdeletion with a novel association with congenital diaphragmatic hernia: a case report. Clin Case Rep 2018;6:592–5. https://doi.org/10.1002/ccr3.1369.Search in Google Scholar PubMed PubMed Central
10. Gelfand, AA, Croen, LA, Torres, AR, Wu, YW. Genetic risk factors for perinatal arterial ischemic stroke. Pediatr Neurol 2013;48:36–41. https://doi.org/10.1016/j.pediatrneurol.2012.09.016.Search in Google Scholar PubMed PubMed Central
11. Ghi, T, Simonazzi, G, Perolo, A, Savelli, L, Sandri, F, Bernardi, B, et al.. Outcome of antenatally diagnosed intracranial hemorrhage: case series and review of the literature. Ultrasound Obstet Gynecol 2003;22:121–30. https://doi.org/10.1002/uog.191.Search in Google Scholar PubMed
Supplementary Material
The online version of this article offers supplementary material (https://doi.org/10.1515/crpm-2021-0064).
© 2022 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Case Reports – Obstetrics
- Chagasic heart failure in a pregnant woman in a non-endemic area: case report and long-term follow-up
- A rare but troublesome complication of cesarean section: the uterocutaneous fistula. Report of two cases and review of literature
- Utilization of point-of-care ultrasound and rotational thromboelastometry (ROTEM) in the diagnosis and management of amniotic fluid embolism presenting as post-partum hemorrhage and cardiac arrest
- Fetal intracranial hemorrhage in a case of 16p microdeletion
- A new sonographic marker in the diagnosis of prenatal bilateral renal agenesis, segmental anterior deviation of the aorta
- Extreme fetal macrosomia at 42 gestational weeks: a case report and literature review
- Acute uterine inversion – A complication revisited; a case series and review of literature
- Prenatal diagnosis of Holt-Oram syndrome
- Hemothorax after fetal pleural effusion-thoracoamniotic shunting procedure due to transient myeloproliferative disorder
- Multimodal postpartum imaging of a severe case of Couvelaire uterus
- Acute glycogenic hepatopathy in pregnancy: a case report and literature review
- Umbilical artery aneurysm without aneuploidy and delivery of a live neonate
- Massive fetomaternal hemorrhage: a case series and review of literature
- Challenges in genetic counseling for congenital anomalies of the kidneys and urinary tract (CAKUT) spectrum
- Anaplastic ganglioglioma in pregnancy a cause of cerebral edema and maternal death
- Prenatal diagnosis of ectrodactyly-ectodermal dysplasia clefting syndrome ‒ a case report with literature review
- Pelvic abscess associated with Actinomyces species ‒ a rare post-cesarean complication
- Haemophagocytic lymphohistiocytosis during pregnancy: a case presentation and literature review
- Autoimmune polyglandular syndrome type 2 in pregnancy: a case report and review of the literature
- Didelphys uterus: a successful induction of labor in a case of intrauterine fetal death near term
- Postpartum sepsis-like illness and rash associated with Hansen’s disease
- Expectant management of placenta accreta after a mid-trimester pregnancy loss: a case report and a short review
- Fetal neonatal alloimmune thrombocytopenia treatment with intravenous immunoglobulin: a challenge in pregnancy management and infection assessment ‒ case report
- Coarctation of the aorta and persistent left superior vena cava: HDlive Flow features at 14 weeks of gestation
- Case Reports – Newborn
- The journey from blue to pink–a rare cause for self-limiting methemoglobinemia in an Indian baby
- Physiological pulmonary assessments in the management of bilateral diaphragmatic eventration
- An unusual case of the congenital mesenchymal hamartoma of the neck associated with the midline cervical cleft in neonate
- Severe hematoma following the use of low molecular weight heparin in preterm neonate
- Neonatal sepsis due to Coxsackievirus B3 complicated by liver failure and pulmonary hemorrhage
- Preterm twins with antenatal presentation of Pearson syndrome
Articles in the same Issue
- Case Reports – Obstetrics
- Chagasic heart failure in a pregnant woman in a non-endemic area: case report and long-term follow-up
- A rare but troublesome complication of cesarean section: the uterocutaneous fistula. Report of two cases and review of literature
- Utilization of point-of-care ultrasound and rotational thromboelastometry (ROTEM) in the diagnosis and management of amniotic fluid embolism presenting as post-partum hemorrhage and cardiac arrest
- Fetal intracranial hemorrhage in a case of 16p microdeletion
- A new sonographic marker in the diagnosis of prenatal bilateral renal agenesis, segmental anterior deviation of the aorta
- Extreme fetal macrosomia at 42 gestational weeks: a case report and literature review
- Acute uterine inversion – A complication revisited; a case series and review of literature
- Prenatal diagnosis of Holt-Oram syndrome
- Hemothorax after fetal pleural effusion-thoracoamniotic shunting procedure due to transient myeloproliferative disorder
- Multimodal postpartum imaging of a severe case of Couvelaire uterus
- Acute glycogenic hepatopathy in pregnancy: a case report and literature review
- Umbilical artery aneurysm without aneuploidy and delivery of a live neonate
- Massive fetomaternal hemorrhage: a case series and review of literature
- Challenges in genetic counseling for congenital anomalies of the kidneys and urinary tract (CAKUT) spectrum
- Anaplastic ganglioglioma in pregnancy a cause of cerebral edema and maternal death
- Prenatal diagnosis of ectrodactyly-ectodermal dysplasia clefting syndrome ‒ a case report with literature review
- Pelvic abscess associated with Actinomyces species ‒ a rare post-cesarean complication
- Haemophagocytic lymphohistiocytosis during pregnancy: a case presentation and literature review
- Autoimmune polyglandular syndrome type 2 in pregnancy: a case report and review of the literature
- Didelphys uterus: a successful induction of labor in a case of intrauterine fetal death near term
- Postpartum sepsis-like illness and rash associated with Hansen’s disease
- Expectant management of placenta accreta after a mid-trimester pregnancy loss: a case report and a short review
- Fetal neonatal alloimmune thrombocytopenia treatment with intravenous immunoglobulin: a challenge in pregnancy management and infection assessment ‒ case report
- Coarctation of the aorta and persistent left superior vena cava: HDlive Flow features at 14 weeks of gestation
- Case Reports – Newborn
- The journey from blue to pink–a rare cause for self-limiting methemoglobinemia in an Indian baby
- Physiological pulmonary assessments in the management of bilateral diaphragmatic eventration
- An unusual case of the congenital mesenchymal hamartoma of the neck associated with the midline cervical cleft in neonate
- Severe hematoma following the use of low molecular weight heparin in preterm neonate
- Neonatal sepsis due to Coxsackievirus B3 complicated by liver failure and pulmonary hemorrhage
- Preterm twins with antenatal presentation of Pearson syndrome

