Abstract
Background
Prenatal diagnosis of congenital ichthyosis is still a challenge and very few cases of sonographic diagnosis have been described in the literature. Diagnosis by fetal ultrasound is made from the late second trimester and prenatal genetic diagnosis can be possible only if a proband is known.
Case presentation
We report the case of a prenatal diagnosis of severe non-syndromic ichthyosis in a primigravida woman with no personal or family history for this pathology.
Conclusion
Our case outlines prenatal sonographic signs suggestive of ichthyosis orienting genetic diagnosis.
Introduction
Congenital ichthyoses are a group of genetic heterogeneous disorders with clinical outcomes of different gravity, from neonatal life-threatening conditions to paediatric delayed onset. They are marked by whitish or brown skin scales of almost the whole body. Very few cases of sonographic prenatal diagnosis have been described in the literature. It is important to be aware of the signs that lead to suspicion as prenatal diagnosis permits an optimal neonatal management.
Congenital ichthyoses can be syndromic or not and their prevalence may vary significantly: from high for common ichthyoses (1:250–1000) to very low as in harlequin ichthyosis (1:300.000) [1]. Different terminologies have been used throughout the years and comparing cases of different authors is not always easy. In 2009, a new classification of the whole ichthyosis was released [1]. Non-syndromic congenital ichthyosis are divided in to the following: common ichthyosis which often has a delayed onset; autosomal recessive congenital ichthyosis (ARCI); keratinopathic ichthyosis (KPI) which are mainly autosomal dominant, except for autosomal recessive epidermolytic ichthyosis (AREI) and five other forms where only the peeling skin disease (PSD) and keratosis linearis ichthyosis congenital keratoderma (KLICK) are autosomal recessive.
We report the case of a prenatal diagnosis of severe non-syndromic ichthyosis in a primigravida woman with no personal or family history for this pathology.
Case presentation
After a normal first trimester ultrasound, a 20-year-old primigravida woman was diagnosed at 27 weeks of gestational age (GA) with fetal growth restriction (FGR). The estimated fetal weight was at the 0.7th percentile. The fetus had facial dysmorphism with the mouth constantly open as an eclabium, hypoplastic nose (Figure 1), intragastric hyperechoic content (Figure 2) and skin scaling with skin particles floating in the amniotic liquid (Figure 3). The amniotic liquid was slightly hyperechoic with sedimentation of skin scales observed by vaginal ultrasound (Figure 4). No visceral abnormality was found. The amniocentesis performed showed an alpha-fetoprotein increased ten-fold (60,500 μg/L). Those findings recall a severe congenital ichthyosis and termination of pregnancy was proposed, but refused. Within several weeks we observed progressively fetal immobilism and hydramnios. At 30 weeks of GA corticosteroids prophylaxis and tocolytics were administrated to prevent premature delivery secondary to uterine contractions due to hydramnios. At 31 weeks of GA the patient gave birth to a baby boy of 1380 g, 40 cm of height and 28 cm of cranial circumference and normal cord blood pH. The Apgar score was 3–3–3. The baby boy had severe ichthyosis, atrophic ears, everted eyelids (ectropion), a hypoplastic nose, eclabium and stiffened skin surface. The couple opted for palliative care and the baby died at 33 min of life. An autopsy was refused. Comparative genomic hybridisation (CGH) array and clinical exome on cord blood were negative.
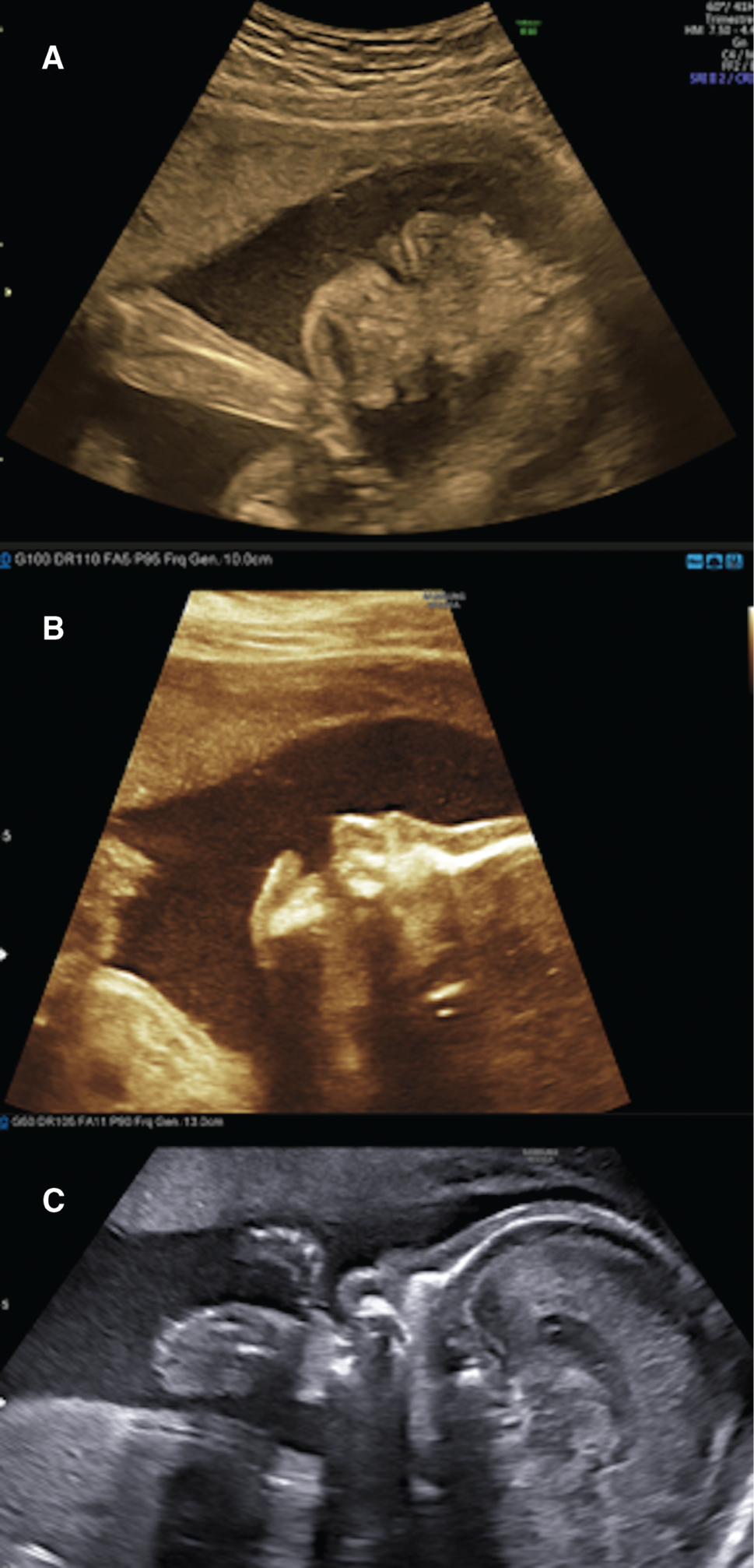
Eclabium and ectropion on the coronal axis of the face; (A) Eclabium and ectropion on the coronal axis of the face; (B) hypoplastic nasal bone and eclabium on the profile view; (C) hypoplastic nasal bone on a strictly median sagittal axis of the head (corpus callosum completely viewed).
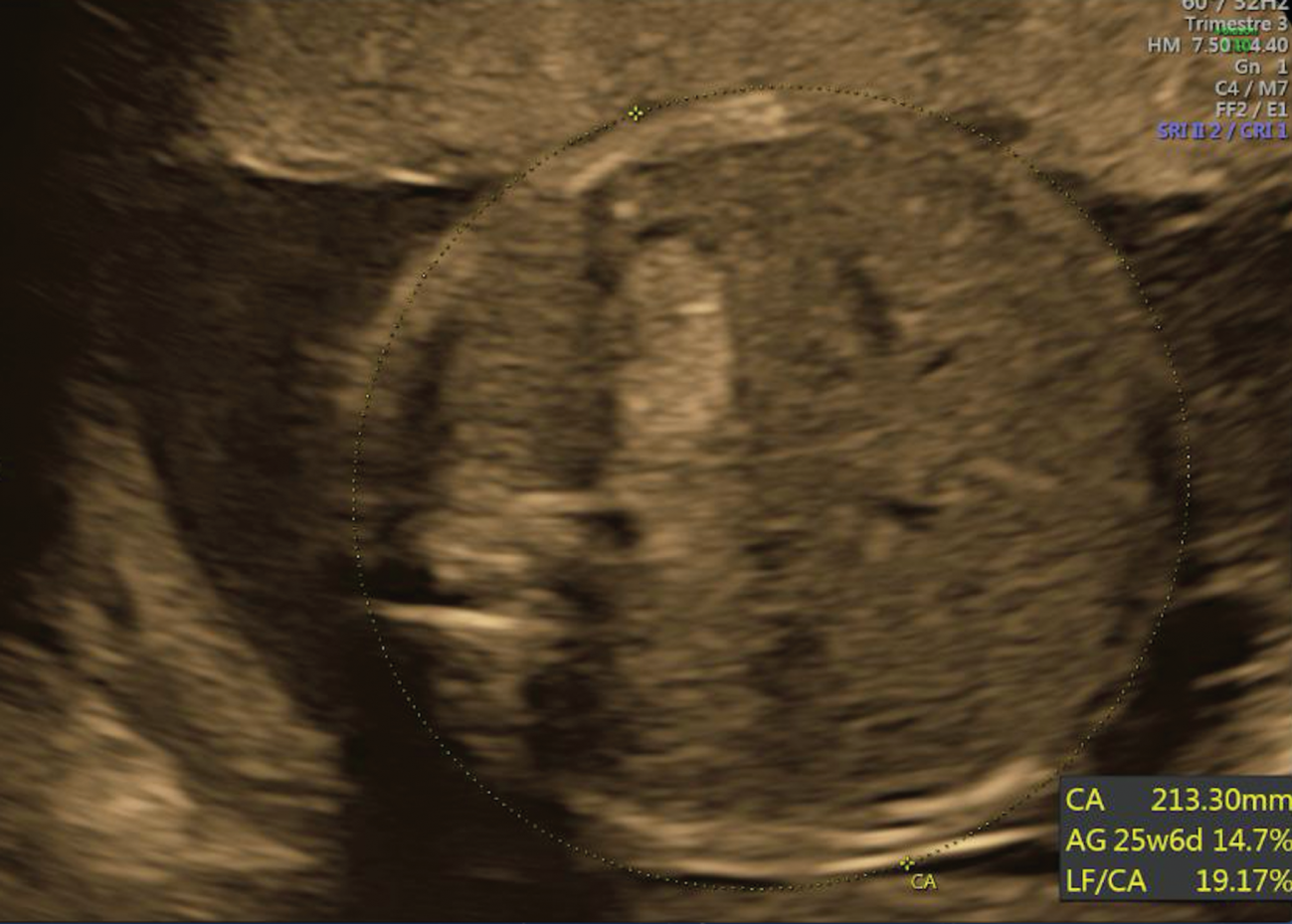
Intragastric hyperechoic image.
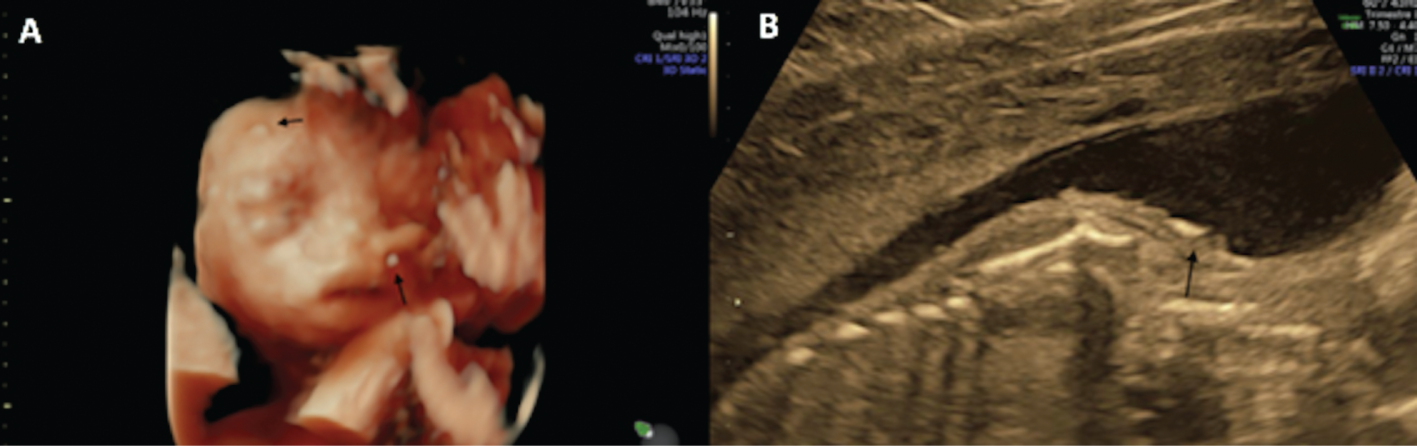
Skin scaling on 3D reconstruction of the face and on the shoulder.
Black arrows on Figure (A) and (B).

Amniotic liquid hyperechoic and skin scales sedimentation observed at vaginal ultrasound, just above the cervix (black arrows).
Ethical considerations
The woman signed an informed consent for genetic analyses and publication.
Discussion
New progress on physiopathology, aetiology and treatment of congenital ichthyosis are constantly being made. However, prenatal diagnosis is still a challenge, partly because abnormalities are visible only in late second and third trimester. This is due to the embryogenesis of fetal skin, which is completed by the 22nd week of GA. Fetal skin biopsies by fetoscopy were performed in the past to make a diagnosis. Nowadays chorionic villus sampling and/or amniocentesis permit a genetic diagnosis, as some causing mutation has been discovered. However not all the implicated genes are known, and even though genetic diagnosis is possible before birth only if a proband is known.
It is therefore important to be aware of the antenatal sonographic signs that lead to suspicion as prenatal diagnosis permits an optimal neonatal management crucial in these newborns. To the best of our knowledge, only 19 other cases of ultrasound prenatal diagnosis of non-syndromic congenital ichthyosis have been described in the literature [2], [3], [4], [5], [6], [7], [8], [9], [10], [11]. They were confirmed at birth either clinically or/and by genetic testing. Our case enriches the literature adding rare and specific sonographic signs.
The most frequent signs found in these articles were FGR, facial dysmorphism with ectropion, eclabium, hypoplastic nose and flattened ears, thick skin, reduced fetal movement with eventually clubfoot, clenched fist and contractures of the limbs. The amniotic liquid was often hyperechoic with a “snowflake sign” due to skin scaling. Polyhydramnios was often associated secondary to fetal immobilism. These signs are concordant with the sonographic presentation of our case.
Some authors [3], [4], [5], [6] used three-dimensional (3D) and four-dimensional (4D) analysis to better visualise the facial dysmorphism. These are diagnostic tools that we recommend using as they helped us to confirm our suspicion, and the parents to better understand the pathology.
We want to underline the presence in our case of an intragastric hyperechoic image, reflection of the skin scales swallowed by the fetus, which is a feature only described once to the best of our knowledge [12]. We consider this as a rare sign that in the presence of other sonographic features could potentially help sonographers in the prenatal diagnosis of congenital ichthyosis.
Prenatal ultrasound besides eventually giving a prenatal diagnosis to parents, has also an important role: preparing neonatologists and intensive care units for an appropriate management of the newborn and further improving parental counselling by a multidisciplinary collaboration.
In conclusion, congenital ichthyosis can be suspected prenatally in case of typical facial dysmorphism, fetal immobilism, FGR, hyperechoic amniotic liquid and intragastric hyperechoic content.
Supplementary informaiton
Supplementary materials: 4 videos.
-
Ethical approval: The research related to human use has complied with all the relevant national regulations, institutional policies and has been conducted in accordance with the tenets of the Helsinki Declaration, and it has been approved by the authors’ Institutional Review Board or equivalent committee.
-
Author contributions: All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
-
Research funding: None declared.
-
Employment or leadership: None declared.
-
Honorarium: None declared.
-
Competing interests: The funding organization(s) played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the report for publication.
References
[1] Oji V, Tadini G, Akiyama M, Blanchet Bardon C, Bodemer C, Bourrat E, et al. Revised nomenclature and classification of inherited ichthyoses: results of the first ichthyosis consensus conference in Soreze 2009. J Am Acad Dermatol. 2010;63:607–41.10.1016/j.jaad.2009.11.020Search in Google Scholar PubMed
[2] Rathore S, David LS, Beck MM, Bindra MS, Arunachal G. Harlequin ichthyosis: prenatal diagnosis of a rare yet severe genetic dermatosis. J Clin Diagn Res. 2015;9:4–6.10.7860/JCDR/2015/15250.6705Search in Google Scholar PubMed PubMed Central
[3] Vohra N, Rochelson B, Smith-Levitin M. Three-dimensional sonographic findings in congenital (Harlequin) ichthyosis. J Ultrasound Med. 2003;22:737–9.10.7863/jum.2003.22.7.737Search in Google Scholar PubMed
[4] Kudla MJ, Timmerman D. Prenatal diagnosis of Harlequin ichthyosis using 3- and 4-dimensional sonography. J Ultrasound Med. 2010;29:317–9.10.7863/jum.2010.29.2.317Search in Google Scholar PubMed
[5] Bongain A, Benoit B, Ejnes L, Lambert JC, Gillet JY. Harlequin fetus: three-dimensional sonographic findings and new diagnostic approach. Ultrasound Obstet Gynecol. 2002;20:82–510.1046/j.1469-0705.2002.00708.xSearch in Google Scholar PubMed
[6] Basgul AY, Kavak ZN, Guducu N, Durukan B, Isci H. Prenatal diagnosis of congenital harlequin ichthyosis with 2D, 3D, and 4D ultrasonography. Clin Exp Obstet Gynecol. 2011;38:283–5.Search in Google Scholar
[7] Zapałowicz K, Wygledowska G, Roszkowski T, Bednarowska A. Harlequin ichthyosis difficulties in prenatal diagnosis. J Appl Genet. 2006;47:195–7.10.1007/BF03194622Search in Google Scholar PubMed
[8] Phadnis SV, Griffin DR, Eady RA, Rodeck CH, Chitty LS. Prenatal diagnosis and management strategies in a family with a rare type of congenital ichthyosis. Ultrasound Obstet Gynecol. 2007;30:908–10. Review.10.1002/uog.4004Search in Google Scholar PubMed
[9] Berg C, Geipel A, Kohl M, Krokowski M, Baschat AA, Germer U, et al. Prenatal sonographic features of Harlequin ichthyosis. Arch Gynecol Obstet. 2003;268:48–51.10.1007/s00404-002-0333-4Search in Google Scholar PubMed
[10] Suresh S, Vijayalakshmi R, Indrani S, Lata M. Short foot length: a diagnostic pointer for harlequin ichthyosis. J Ultrasound Med. 2004;23:1653–7.10.7863/jum.2004.23.12.1653Search in Google Scholar PubMed
[11] Holden S, Ahuja S, Ogilvy-Stuart A, Firth HV, Lees C. Prenatal diagnosis of Harlequin ichthyosis presenting as distal arthrogryposis using three-dimensional ultrasound. Prenat Diagn. 2007;27:566–7.10.1002/pd.1727Search in Google Scholar PubMed
[12] Blaas HG, Salvesen KÅ, Khnykin D, Jahnsen FL, Eik-Nes SH. Prenatal sonographic assessment and perinatal course of ichthyosis prematurity syndrome. Ultrasound Obstet Gynecol. 2012;39(4):473–7.10.1002/uog.9014Search in Google Scholar PubMed
Supplementary Material
The online version of this article offers supplementary material (DOI: https://doi.org/10.1515/crpm-2018-0048).
© 2019 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Case Reports – Obstetrics
- Large placental chorioangioma: a potential effective in-utero treatment modality for radio frequency ablation
- Prenatal diagnosis of fetal hemivertebra in the first trimester
- Congenital cytomegalovirus infection presenting as a fetal intra-abdominal cyst
- Surgical prophylaxis of bleeding during an the operative delivery in a patient with HELLP syndrome
- Modified surgical technique in an unusual uterine rupture
- Typical changes of ethmocephaly and holoprosencephaly in a fetus at 14 weeks of gestation
- Sudden severe fetal compromise at a planned home birth – a case of umbilical cord prolapse
- Vaginal delivery after laparotomic myomectomy during pregnancy
- Recurrent pleural effusion and pain in the shoulder in women of reproductive age could have a gynecological cause: case series
- Comprehensive antenatal to postpartum care of patient with bipolar disorder: a case report
- An ethical framework for counseling about mode of delivery for desired psychosocial benefit in pregnancies complicated by severe fetal anomalies
- Legionella infection in pregnancy: imitator of HELLP syndrome, presenting as acute respiratory failure and septic shock
- Case Reports – Fetus
- Postnatal outcomes of babies diagnosed with hydronephrosis in utero in a tertiary care centre in India over half a decade
- Ovarian torsion of a term pregnancy – a new twist: review of the literature and management
- Severe congenital non-syndromic ichthyosis: ultrasound diagnosis of a prenatal case
- Maternal Graves’ disease and fetal tetralogy of Fallot: a case series
- Case Reports – Newborn
- Inefficiency of levothyroxine suspension in a neonate with congenital hypothyroidism
- Segmental absence of intestinal musculature in an extremely low birthweight preterm infant
- Neonatal hyperbilirubinaemia necessitating exchange transfusion due to maternal sickle cell crisis
- Central edema in critically ill neonates
Articles in the same Issue
- Case Reports – Obstetrics
- Large placental chorioangioma: a potential effective in-utero treatment modality for radio frequency ablation
- Prenatal diagnosis of fetal hemivertebra in the first trimester
- Congenital cytomegalovirus infection presenting as a fetal intra-abdominal cyst
- Surgical prophylaxis of bleeding during an the operative delivery in a patient with HELLP syndrome
- Modified surgical technique in an unusual uterine rupture
- Typical changes of ethmocephaly and holoprosencephaly in a fetus at 14 weeks of gestation
- Sudden severe fetal compromise at a planned home birth – a case of umbilical cord prolapse
- Vaginal delivery after laparotomic myomectomy during pregnancy
- Recurrent pleural effusion and pain in the shoulder in women of reproductive age could have a gynecological cause: case series
- Comprehensive antenatal to postpartum care of patient with bipolar disorder: a case report
- An ethical framework for counseling about mode of delivery for desired psychosocial benefit in pregnancies complicated by severe fetal anomalies
- Legionella infection in pregnancy: imitator of HELLP syndrome, presenting as acute respiratory failure and septic shock
- Case Reports – Fetus
- Postnatal outcomes of babies diagnosed with hydronephrosis in utero in a tertiary care centre in India over half a decade
- Ovarian torsion of a term pregnancy – a new twist: review of the literature and management
- Severe congenital non-syndromic ichthyosis: ultrasound diagnosis of a prenatal case
- Maternal Graves’ disease and fetal tetralogy of Fallot: a case series
- Case Reports – Newborn
- Inefficiency of levothyroxine suspension in a neonate with congenital hypothyroidism
- Segmental absence of intestinal musculature in an extremely low birthweight preterm infant
- Neonatal hyperbilirubinaemia necessitating exchange transfusion due to maternal sickle cell crisis
- Central edema in critically ill neonates


