From automation to agentic artificial intelligence in laboratory medicine: an opinion of the IFCC Division on Emerging Technologies
-
Damien Gruson
, Bernard Gouget
, Woochang Lee
Abstract
Agentic artificial intelligence (AI) systems are distinguished by their ability to invoke multiple tools, compose command chains, and combine chain-of-thought reasoning with deep research to execute complex tasks and take actions. This represents a major evolution beyond machine learning and large language models (LLM), toward systems capable of planning, executing, and coordinating complex workflows. In contrast to traditional LLMs, which primarily focus on generating and classifying information, agentic AI introduces elements of autonomy, reasoning, and orchestration, while digital twins extend this concept to dynamic virtual representations of patients and laboratory processes, capable of continuous learning, simulation and adaptation. This transition has profound implications for laboratory medicine, a field characterized by high data complexity, multi-omics integration, and stringent operational demands. At the same time, laboratories face growing expectations regarding efficiency, resource stewardship, and value-based healthcare delivery. This article explores both the opportunities and limitations of agentic AI in laboratory medicine, highlighting its potential to move beyond static automation toward autonomous, outcome-driven innovation. It also examines the ethical, interpretability, and governance considerations that must accompany its implementation.
Introduction
Artificial intelligence (AI) has rapidly become a cornerstone of healthcare research and practice. In laboratory medicine, applications of machine learning and large language models (LLMs) have already demonstrated promise in diagnostics, clinical decision support, and workflow optimization [1], 2]. While these AI systems can generate valuable insights and recommendations, they still depend on human users to interpret and implement their outputs.
Agentic AI represents a fundamental shift in this paradigm. Unlike traditional models that stop at prediction, agentic systems can reason, plan, and act autonomously across multiple steps of a process. Digital twins complement this evolution by creating dynamic, continuously updated virtual replicas of laboratory systems or patient trajectories, bridging the gap between simulation and real-world practice. By combining task decomposition, decision-making, and orchestration of diverse digital tools, agentic AI functions less like a passive assistant and more like a “digital colleague” [3]. This emerging framework extends traditional AI capabilities by integrating chain-of-thought reasoning, deep research, multimodal tool orchestration, and autonomous execution.
In the laboratory context, this evolution is particularly transformative. Agentic AI has the potential to move beyond static automation and data reporting, enabling laboratories to operate as adaptive ecosystems that deliver continuous, outcome-driven value. For instance, consider the common goal of releasing a safe and timely troponin result: an agentic AI could autonomously query the laboratory informatics system (LIS), middleware, and electronic health records (EHR); retrieve historical results, instrument status, and standard operating procedures; route the specimen via total laboratory automation; apply test-use rules; validate and generate structured reports; interpret results with follow-up recommendations; and escalate unusual findings to staff.
Preliminary studies indicate that this architecture may outperform baseline LLMs in clinical tasks by leveraging structured reasoning and tool orchestration [4], 5]. However, the transition from assistance to autonomy also intensifies the need for interpretability, transparency, and clearly defined human oversight (“human in the loop”) to ensure accountabilities for all automated actions.
From automation to agentic AI in laboratory medicine
Laboratories have long embraced automation, from robotic pipetting to total laboratory automation platforms. These systems, however, follow rigid pre-programmed rules and cannot adapt in real time to clinical or operational variability. Agentic AI could extend beyond this limitation by dynamically managing the entire testing cycle: verifying the appropriateness of test requests, optimizing sample routing, validating results, and autonomously drafting structured reports directly linked to electronic health records [6].
Multi-modal integration is another frontier. Laboratory medicine is increasingly tasked with managing diverse layers of information: genomics, proteomics, metabolomics, and exposome data. Traditional AI models often struggle with this heterogeneity, but agentic AI can navigate complexity by retrieving literature, linking datasets, and generating adaptive insights [1], 7].
For example, in cardiovascular prevention, continuous integration of exposome data with genetic and metabolic information could enable personalized and dynamic risk models. Such integration would bring laboratories closer to the concept of a patient-specific digital twin, where real-time biomarker data inform adaptive clinical pathways. Nevertheless, while early demonstrations such as Biomni illustrate the potential of biomedical agent frameworks, they remain at the preprint stage and require independent validation, robust reproducibility assessment, and contextual adaptation before being generalized to clinical laboratory environments. Such advances would allow laboratory medicine to move from reactive testing toward proactive, longitudinal health management (Figure 1).
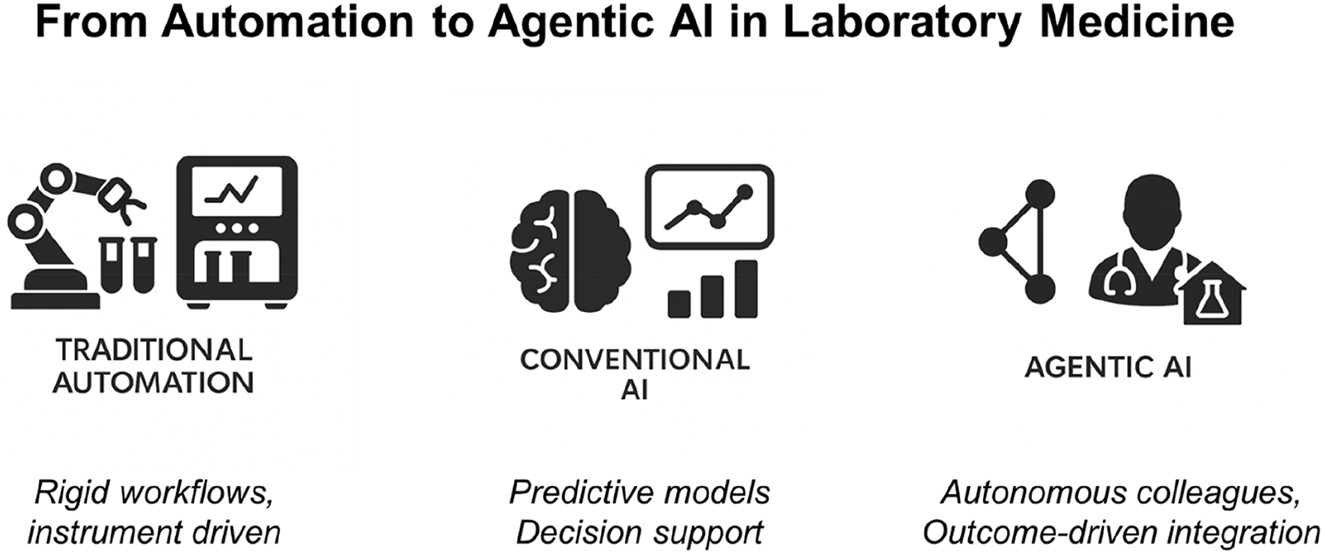
From automation to agentic AI in laboratory medicine. Schematic illustrating three progressive stages – traditional automation, conventional AI, and agentic AI – highlighting the transition from fixed workflows to intelligent decision support, and ultimately autonomous digital colleagues. Although conceptual in nature, the figure illustrates a continuum of automation maturity and serves as a visual framework for contextualizing future developments.
Agentic AI in biomedical research
Agentic AI is also reshaping biomedical research. The concept of “self-driving laboratories” illustrates how AI agents can autonomously generate hypotheses, analyze outputs, and refine protocols without direct human intervention. Platforms such as Biomni demonstrate the feasibility of a generalist biomedical agent capable of handling genomics, microbiome analysis, and wearable sensor data [7]. However, this example must be interpreted with caution as it is based on an early, non-peer-reviewed study, and the actual implementation of pathway-reasoning and causal modeling remains limited.
Applied to laboratory medicine, such systems could accelerate biomarker discovery and validation, democratize access to advanced analyses, and shorten the translational pipeline from research to clinical practice [6]. Yet these benefits will depend on rigorous validation, strong ethical governance, and careful adaptation to the technical and regulatory context of each laboratory.
Stewardship and value-based care
Another crucial aspect is stewardship and value-based medicine. Laboratory medicine plays a pivotal role in healthcare cost-effectiveness. By monitoring appropriateness, preventing redundant testing, and linking test use to clinical outcomes, agentic AI could strengthen the laboratory’s contribution to value-based healthcare [8]. Such systems could act as safeguards of diagnostic appropriateness, ensuring that tests ordered are clinically justified, results are properly contextualized, and resources are used responsibly.
However, interpretability remains a key limitation. While rule-based and classical ML systems offer transparent logic, agentic AI operates through dynamic decision graphs and multitools orchestration making traceability more challenging. This opacity necessitates audit logs, model explainability modules, and human supervision to ensure ethical and legal accountability. The “human in the loop” paradigm must remain central, as responsibility ultimately lies with the professional overseeing the agentic process. This aligns directly with the increasing pressure on healthcare systems to optimize both outcomes and costs. By embedding interpretable, auditable and trustworthy architectures, agentic AI can help laboratories uphold both efficiency and trust, while maintaining the stewardship values that underpin clinical biochemistry.
Challenges and governance
Despite this promise, several challenges remain. Laboratory data present unique complexities absent from many other healthcare domains: analyte variability, method dependency, and metadata requirements. The European Federation for Laboratory Medicine (EFLM) checklist highlights the importance of harmonization, explicit reporting of pre-analytical conditions, and rigorous validation for AI in laboratory settings [2]. Without such safeguards, agentic systems risk generating non-transferable or non-reproducible models.
Trust, ethical governance, and regulatory clarity also pose major concerns. Agentic AI systems operate autonomously and may interact with critical infrastructures; therefore, governance frameworks must proactively address scenarios of liability, data drift, and unintended actions. Ethical oversight should ensure compliance with principles of beneficence, non-maleficence, autonomy, and justice, particularly as regulatory frameworks such as emerging regulatory instruments such as the EU AI Act continue to evolve [9].
Transparency demands adherence to FAIR principles (Findable, Accessible, Interoperable, Reusable), as well as a commitment to reproducibility, and strong governance practices. Integrating AI assurance frameworks, systematic bias monitoring, and continuous post-deployment performance validation will be essential to foster trust and enable sustainable adoption.
Finally, human factors must be considered. Laboratory professionals will need to evolve into supervisors of autonomous systems, ensuring oversight, exception management, and ethical responsibility [3]. Education and training will therefore be key to a safe and effective transition.
Outlook
Looking ahead, laboratories can start small, deploying agentic AI for targeted tasks such as test stewardship, appropriateness monitoring, or automated reporting. Over time, integration with laboratory information systems and electronic health records will allow orchestration across disciplines.
Concrete pilot projects already provide insights into how such systems could operate in practice. For example, in thyroid disease management, inappropriate ordering of free hormone tests (FT4 and FT3) remains a major challenge in primary care. Reinforcing a reflexive algorithm in the Saskatoon Health Region reduced unnecessary FT4 and FT3 testing by 40–60 %, with significant cost savings and better alignment with guidelines [10]. This was achieved through a conventional rule-based approach; in contrast, an agentic AI could build upon such logic by autonomously enforcing test algorithms across systems, while preserving human interpretability and ensuring contextual validation.
Another proof-of-concept comes from cardiovascular research, where spatial transcriptomic analyses in heart failure have revealed novel biomarkers such as CRIP3, PFKFB2, and TAX1BP3, as well as endothelial subclusters driving fibrosis and inflammation [11]. In a self-driving laboratory framework, agentic AI could autonomously design and refine experimental workflows – integrating multi-omics (spatial transcriptomics, proteomics, metabolomics) with clinical outcomes – and iteratively validate these candidate biomarkers. Platforms such as Biomni [7] and agentic models for scientific discovery already demonstrate feasibility [6]. Applied to heart failure, such systems could accelerate the translation of molecular insights into clinically actionable diagnostics and prognostic tools. However, these approaches must remain grounded in robust empirical validation and clearly defined, transparent decision pathways.
Ultimately, laboratories may evolve into adaptive ecosystems where human professionals and digital colleagues work in tandem, continuously optimizing diagnostics, workflows, and research. These examples underscore that the challenge ahead lies not in technological capability but in responsible, context-aware implementation within the laboratory setting. With proper governance, strong interpretability safeguards, and interdisciplinary collaboration, agentic AI can augment – rather than replace – human expertise.
Conclusions
Agentic AI is not merely a technological upgrade but a catalyst for the reinvention of laboratory medicine. By moving beyond smart tools toward autonomous digital colleagues, it empowers laboratories to transcend their traditional role and fully embrace value creation in healthcare. Its ultimate impact will depend on how effectively it advances patient outcomes, optimizes cost-effectiveness, and supports sustainability across healthcare systems. With aligned governance frameworks and ongoing validation, agentic AI can strengthen the laboratory’s role as a trusted, adaptive, and value-generated partner in the evolving healthcare ecosystem.
-
Research ethics: Not applicable.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Competing interests: The authors state no conflict of interest.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. Gruson, D, Öz, TK. Trends in healthcare and laboratory medicine: a forward look into 2025. Balkan Med J 2025;42:487. https://doi.org/10.4274/balkanmedj.galenos.2025.2024-12-133.Search in Google Scholar PubMed PubMed Central
2. Carobene, A, Cadamuro, J, Frans, G, Goldshmidt, H, Debeljak, Z, De Bruyne, S, et al.. EFLM checklist for the assessment of AI/ML studies in laboratory medicine: enhancing general medical AI frameworks for laboratory-specific applications. Clin Chem Lab Med 2025;64:27–40. https://doi.org/10.1515/cclm-2025-0841.Search in Google Scholar PubMed
3. Lakhan, SE. The agentic era: why biopharma must embrace artificial intelligence that acts, not just informs. Cureus 2025;17:e83390. https://doi.org/10.7759/cureus.83390.Search in Google Scholar PubMed PubMed Central
4. Gorenshtein, A, Omar, M, Glicksberg, BS, Nadkarni, GN, Klang, E. AI agents in clinical medicine: a systematic review. medRxiv 2025. https://doi.org/10.1101/2025.08.22.25334232.Search in Google Scholar PubMed PubMed Central
5. Barra, FL, Rodella, G, Costa, A, Scalogna, A, Carenzo, L, Monzani, A, et al.. From prompt to platform: an agentic AI workflow for healthcare simulation scenario design. Adv Simul 2025;10:1–9. https://doi.org/10.1186/s41077-025-00357-z.Search in Google Scholar PubMed PubMed Central
6. Hartung, T. AI. Agentic models and lab automation for scientific discovery – the beginning of scAInce. Front Artif Intell 2025;8:1649155. https://doi.org/10.3389/frai.2025.1649155.Search in Google Scholar PubMed PubMed Central
7. Huang, K, Zhang, S, Wang, H, Qu, Y, Lu, Y, Roohani, Y, et al.. Biomni: a general-purpose biomedical AI agent. bioRxiv 2025. https://doi.org/10.1101/2025.05.30.656746.Search in Google Scholar PubMed PubMed Central
8. Plebani, M, Cadamuro, J, Vermeersch, P, Jovičić, S, Ozben, T, Trenti, T, et al.. A vision to the future: value-based laboratory medicine. Clin Chem Lab Med 2024;62:2373–87. https://doi.org/10.1515/cclm-2024-1022.Search in Google Scholar PubMed
9. Gruson, D, Gruson, D, Macq, B. The next clinical decision Frontier: how to efficiently and safely combine machine learning and human expertise. Clin Chem 2024;70:471–3. https://doi.org/10.1093/clinchem/hvad155.Search in Google Scholar PubMed
10. Murthy, S, Scott, J, Lu, S, Zhang, D, Vanstone, JR, Berry, WE, et al.. Reducing unnecessary free thyroid hormone testing by the reinforcement of a reflexive algorithm in an outpatient environment. Clin Biochem 2025;137:110919. https://doi.org/10.1016/j.clinbiochem.2025.110919.Search in Google Scholar PubMed
11. Lee, SE, Joo, JH, Hwang, HS, Chen, SF, Evans, D, Lee, KY, et al.. Spatial transcriptional landscape of human heart failure. Eur Heart J 2025;46:3098–114. https://doi.org/10.1093/eurheartj/ehaf272.Search in Google Scholar PubMed PubMed Central
© 2025 Walter de Gruyter GmbH, Berlin/Boston

