Abstract
Background
A large number of psychotropic drugs can interfere with the thyroid physiology, function and autoimmunity.
Objective
The aim of the present study was to investigate the effects of alprazolam and haloperidol on thyroglobulin, antithyroglobulin (aTg), antithyroid peroxidase, and thyroid stimulating hormone levels on rats.
Materials and Methods
First group of adult male Wistar rats was the control, second group received 0.5 mg kg−1 haloperidol in physiological saline and the third group received 0.5 mg kg−1 alprazolam, via gastric gavage once daily for 28 days. Plasma levels of all thyroid function tests were measured with chemiluminescent assay.
Results
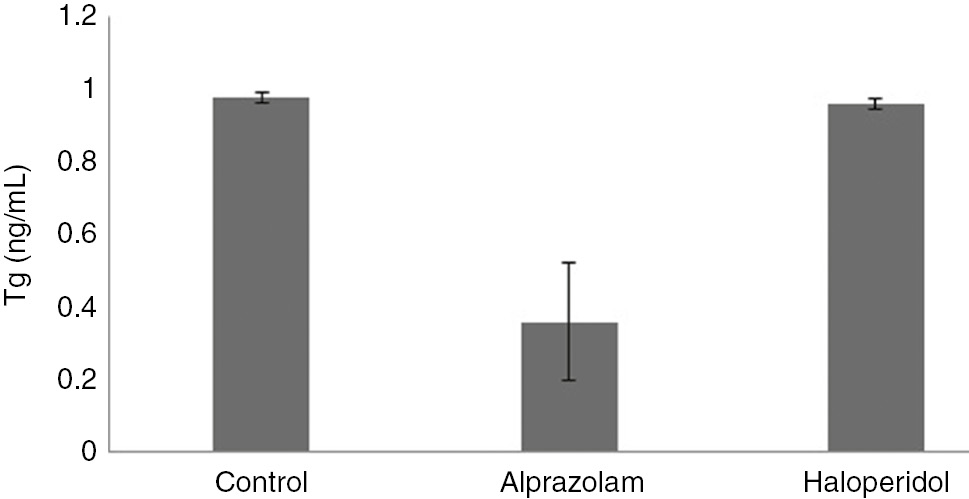
We have investigated a decrease in aTg amounts of control group (5.461±0.718) compared with drug treated rats with alprazolam (1.433±0.225) and haloperidol (1.21±0.228). (PaTg=0.00[ALP], PaTg=0.01[HAL]). Although there were not any change in thyroglobulin levels in the haloperidol treated groups (0.9583±0.014) relative to control group (0.975±0.015); but in opposition Tg levels decreased significantly in response to alprazolam (0.36±0.16) compared with the control group (0.975±0.015), p-values are (PTg=0. 001[ALP]), (PTg=0. 021[HAL]).
Conclusion
We found that these two drugs may interfere with the thyroid physiology and metabolism.
Özet
Amaç
Psikotropik ilaçların büyük bir kısmı tiroit fizyolojisi, fonksiyonu ve otoimmünitesi üzerine etki edebilir. Alprazolam ve haloperidol’un sıçan tiroglobulin (Tg), antitiroglobulin (aTg), antitiroid peroksidaz (TPO), ve tiroid stimüle edici hormon (TSH) üzerine etkilerinin araştırılması bu çalışmanın amacıdır.
Materyal ve Metot
Hayvanlar üç gruba ayrıldı: birinci gruba kontrol grubu olarak fizyolojik salin, ikinci gruba fizyolojik salin içinde 0,5 mg kg−1 haloperidol, üçüncü gruba ise 0,5 mg kg−1 alprazolam 28 gün süre ile günde bir kez gastrik gavage yoluyla ilaç verildi. Plazmada tiroglobülin antitiroglobulin, antitiroid peroksidaz ve tiroid uyarıcı hormon düzeyleri kemiluminesant yöntemi ile ölçüldü.
Bulgular
Haloperidol (1,21±0,228) ve alprazolam (1,433±0,225) ile tedavi edilen sıçanların aTg düzeyleri kontrol grubu (5,461±0.718) ile karşılaştırıldığında, önemli bir ölçüde azalma olduğu gözlendi. (PaTg=0,00[ALP], PaTg=0,01[HAL]). Haloperidol ile tedavi edilen grubun Tg düzeyi (0,9583±0,014) kontrol grubu ile karşılaştırıldığında (0,975±0,015) önemli bir değişiklik gözlenmezken, alprazolam ile tedavi edilen grupta (0,36±0,16), önemli ölçüde azalma saptandı P değerleri, (PTg=0,001 [ALP]), (PTg=0,021 [HAL]).
Sonuç
Bizim bulgularımıza göre bu iki psikotrop ilaç tiroid fizyoloji ve metabolizmasını etkileyebilir.
Introduction
Antipsychotic drugs have been used for the treatment of psychotic disorders and agitated mental disorders since the mid1950s [1]. A large number of psychotropic drugs, anticonvulsants, non-steroidal anti-inflammatory drugs, beta-adrenoceptor antagonists and antiepileptic drugs can increase of thyroid-stimulating hormone (TSH) and decrease of free triiodothyronine thyroid hormone (TH) secretion and may cause induction of autoimmune hypothyroidism or hyperthyroidism. These drugs affect the transport, metabolism, action and excretion of T4 or inhibit thyroid peroxidase activity, enhance deiodination of T4 to T3 or affect iodine capture by thyroid cells [2], [3], [4], [5], [6], [7], [8]. As antipsychotics and tranquilizer drugs are administered over long periods, clinicians need to be aware of possible outcomes, adverse effects in various diseases [9], [10]. Thyroid abnormalities occur frequently in patients with psychotic syndromes thus, patients should be regularly tested in clinical or subclinical thyroid abnormalities on all drug therapies to prevent adverse effects [11].
Alprazolam; 8-chloro-1-methyl-6-phenyl-4H-[1], [2], [4] triazolo [4,3-a] benzodiazepine is a widely prescribed short-acting benzodiazepine which is used in the management of anxiety disorders especially used in panic disorder. This drug belongs to the class of anxiolytic, sedative and hypnotic anticonvulsant which is one of the most commonly used antidepressant [1], [3], [12]. Alprazolam rapidly reduces the symptoms of anxiety, however, the overuse of benzodiazepines was shown to have adverse effects [3]. Compared with other benzodiazepines, alprazolam has short half-life, and high binding affinity to the GABA receptor, and a rapid onset of action [12], [13], [14]. In a previous study, researchers evaluated effects of alprazolam on hamsters and found out that there are important effects of this drug on thyroid function [15]. Haloperidol is a butyrophenone and dopamine antagonist typical neuroleptic agent characterized as a high effective antipsychotic used in the treatment of schizophrenia and its’ used to alleviate care of many syndromes, such as nausea, vomiting and delirium [16], [17]. This drug is often associated with various metabolic side effects [18]. In a previous study which was done on male schizophrenic patients, haloperidol had some effects on TSH responses. The researchers pointed out that TSH releasing actions of TRH are not mediated via receptors that are effectively blocked by haloperidol [19]. Haloperidol has roles in free radical involvement, thus leading to neurodegeneration and these side effects appointed during and after administration of the drug. The neurotoxic metabolites of this drug may have an obscure role in the neurodegenerative diseases [10], [16]. The thyroid plays a significant role in cognition. Disorders of the thyroid have been investigated in Alzheimer’s disease and neuropsychiatric behaviors [20], [21]. Hypothyroidism and subclinical hyperthyroidism have both been associated with cognitive impairment and dementia and elderly patients with cognitive impairment should always be assessed for hypothyroidism [22].
Studies in the field of molecular mechanisms and role of enzymes help us to provide a better understanding of the both cascade of biochemical events that occurs with the effects of the mentioned drugs on thyroglobulin, antithyroglobulin, antithyroid peroxidase and TSH [23]. Thyroidal disorder evaluation in antipsychotic medicated patients presents a particular challenge [10]. These findings made us promptly to explore the effect of alprazolam and haloperidol on some thyroidal factors. We examined the effects of alprazolam and haloperidol treatment on thyroglobulin, antithyroglobulin, thyroid peroxidase, anti-thyroid peroxidase and TSH in rats. Thyroidal disorder assessment in antipsychotic medicated patients presents a particular challenge. This made us promptly to investigate the effect of alprazolam and haloperidol on some thyroidal factors.
Materials and methods
Male Wistar rats, body weight 250–300 g were fed a standard rat chow diet with ad libitum access to food and water. They were housed individually in filter-top standard cages and they were situated in ventilated soundproof boxes. They were kept in a temperature and humidity controlled (22–24°C) animal room, with an alternating light-dark cycle with the lights going on at 7:00 a.m. (12 h light: 12 h dark schedule). A stock solution of haloperidol (Sigma Chemicals, St Louis, MO, USA) was prepared by heating haloperidol in 10 mL 1% lactic acid until dissolved. To obtain solutions of 0.5 mg/mL haloperidol, the stock solution was diluted with distilled water.
Alprazolam (Sigma Chemicals) was prepared daily by dissolving 140 mg of alprazolam in 0.5 mL of 1 N HCl with gentle heating, then diluting the solution with distilled water to 0.5 mg/mL. After an adaptation period of 1 h and examination of the rats we started to give the drugs by means of oral gavage. All experiments were started at the same time of the day (8.00 a.m.). The animals received drugs orally daily with gastric gavage during 28 days. Bloods were collected by a direct cardiac puncture. After centrifugation of the blood samples, the isolated plasma analyzed and measured automatically by the chemiluminescence Immuno Assay (CLIA) method, (LIAISON Immunoassay, DIA Sorin S.P.A Italy) and its special kits for this set.
This study was performed in Urmia University, Faculty of Medicine, department of medical Biochemistry.
All research and animal care procedures were conducted in conformity with international laws and policies. All the animals used for in our experiments were carried out in compliance with EU legislation. (EEC Council Directive 86/609, OJ L 358, I, Dec.12, 1987; Guide for the Care and Use of Laboratory Animals, US National Research Council, 1996). The rats anesthetized by ether. Bloods were collected by direct cardiac puncture. All efforts were made to minimize animal suffering and reduce the number of animals used.
Statistical evaluation
Statistical evaluation was performed using ANOVA followed by the Tukey HSD and Dunnett T3 for our data. A p-value less than p<0.05 was defined to be statistically significant. The data are expressed as mean±standard deviation (SD).
Results
Effects of alprazolam (Figure 1A) [24] and haloperidol [25] (Figure 1B) on thyroglobulin, antithyroglobulin, antithyroid peroxidase and TSH levels were studied. Six male rats were in each group. The animals were assigned randomly into three main experimental groups. According to the treatments they were divided into three groups; group 1 or control group, no drug or placebo, received control serum normal saline 0.9% 2 mL per rat; the second group received serum normal saline 0.9% 2 mL per rat +0.5 mg kg−1 haloperidol; the third group, received serum normal saline 0.9%, 2 mL per rat +0.5 mg kg−1 alprazolam. This dose regimen was chosen to emulate the therapeutic range of doses given to patients and was shown to be effective in other behavioral and biochemical studies. There are a few animal models studies have been done in understanding the mechanism of action of antipsychotic drugs and the doses have been often chosen for haloperidol 0.5 mg/kg, 1 mg/kg and 2 mg/kg, respectively [26], [27], [28], and for alprazolam were 0.3 mg/kg 2 and 4 mg/kg [29], [30].

(A) Schematic structure of Alprazolam. (B) Schematic structure of Haloperidol.
The results of the control group in comparison with treated groups showed that these drugs have not any significant change and effect on TSH. According to p<0.05, the amounts of these drugs in relation with this hormone is (p TSH=0.99[ALP], p TSH=1.00 [HAL]) (Figure 2). Accordingly, there were not any significant change in the haloperidol treated group; however, Tg levels decreased significantly in response to alprazolam (Figure 3). Under treatment with haloperidol, p=0.21 gained for Tg thus there is not any significant change, but there are significant changes in Tg amounts under treatment with alprazolam (p=0.001).

Effects of alprazolam and haloperidol on TSH.
Effects of alprazolam and haloperidol on Tg.
We found that antithyroglobulin levels decreased significantly in drug treated rats compared with control group (Figure 4). P aTg=0.00 gained for aTg after treatment with these drugs showed significant changes (p<0.05). According to these amounts (p aTPO=0.73[AlP], p aTPO=0.94[HAL]), there were not any statistically significant differences in aTPO levels in response to treatment with alprazolam and haloperidol (Figure 5). Thyroglobulin levels, did not change significantly in haloperidol treatment group; however, Tg levels decreased significantly in response to alprazolam (Figure 2). We have also shown the results of the control group in comparison with drug treated groups (Table 1).

Effects of alprazolam and haloperidol on aTg.

Effects of alprazolam and haloperidol on aTPO.
The results of control group in comparison with drug treated groups.
| Variables | Control | Alprazolam | Haloperidol | p-Value |
|---|---|---|---|---|
| TSH (mIU/mL) | 0.012±0.001 | 0.012±0.001 | 0.012±0.001 | p>0.05 |
| aTg (IU/mL) | 5.461±0.718 | 1.433±0.225a | 1.210±0.228a | p<0.05 |
| aTPO (IU/mL) | 0.108±0.007 | 0.123±0.038 | 0.112±0.014 | p>0.05 |
| Tg (ng/mL) | 0.975±0.015 | 0.360±0.160a | 0.958±0.014 | p<0.05 |
aDenotes statistical significance of control subjects (p<0.05). Variables showed Mean±SD.
Discussion
As antipsychotics and tranquilizer drugs are administered over long periods in humans, their possible endocrine toxic effects and adverse outcomes must be taken into consideration [9]. According to our study there are some changes in the amount of Tg after treating with alprazolam and haloperidol. Increased levels of serum Tg and aTg is associated with thyroid disorders such as Graves’ disease, toxic adenoma, nontoxic goiter and subacute thyroiditis. We observed, decreasing amount of Tg after treatment with alprazolam and haloperidol. Accordingly, these drugs may be an alternative use for treatment of some thyroid diseases as well as we saw increasing levels of serum Tg and aTg [31]. According to studies antipsychotic medicated patients, frequently present thyroid function disorders such as hypothyroidism and thyroid abnormalities [32], [33], [34], [35], [36]. It has been suggested that the most consistent findings derive from antipsychotic medicated patients, in whom serum levels of TSH seem to be reduced, although still within the normal ranges [37]. Furthermore, it has been also demonstrated by various researchers that antidepressant treatment results in thyroid hormones without a significant reduction in TSH [19], [38]. Our study results are consistent with these studies. In another study Robertas and Prange confirmed significant changes on thyroid after psychotropic therapy [7]. It is important to keep in mind that a few drugs, are associated with the development of clinically significant thyroid disease [39]. These psychotropic medications are frequently administered especially for adults. Consumption of these drugs is associated with potentially serious side effects [40]. Thyroidal disorder evaluation in antipsychotic medicated patients presents a particular challenge. Many psychotropic compounds interfere with the thyroid physiology as a result of their action on many levels [41], [42]. Animal studies have shown that treatment with antipsychotics, like haloperidol is associated with changes in the expression of nuclear receptors and genes involved in thyroid hormone function [43]. For management of any thyroid disorders that can happen for patients medicated with these drugs, understanding the effects of every class of drugs is very important.
Psychotic drugs may affect thyroid function in various aspects and this problem may be more serious in elderly patients. They showed that treatment with alprazolam decreased the T3 concentration in serum, but it was not any significant change on T4 [15]. We demonstrate that treatment with alprazolam decreased the amount of Tg. According to these results, alprazolam changed the amount of Tg and T3, but did not have any effects on T4. Because Tg is the main and essential factor for the synthesis of thyroid hormones and it is their precursor, so any changes in Tg amount, might cause some changes in the thyroid gland. A similar conclusion was reached by Baumgartner et al. [44] that thyroid function may be altered as a direct consequence of antipsychotic drug treatment On the other hand, psychotic drugs such as haloperidol associated with diagnoses of thyrotoxicosis [45].
Therefore, consumption of these drugs might cause some disease and disorders of the thyroid gland and this hypothesis require more researches.
Conclusion
Over the years, several drugs used in the treatment of nonthyroidal conditions have been shown to affect thyroid function and metabolism. Some of the interactions of antipsychotic drugs with thyroid function have already been explained but mechanisms remains to be demonstrated. Psychotic drugs may affect thyroid function in numerous ways and they can cause different abnormalities. In addition to common side effects, many drugs cause dangerous side effects and patients receiving these drugs should be screened for thyroid function abnormalities regularly after drug initiation. Above all, the relationship between the thyroid and some psychoactive drugs is generally unknown. Taken together, these data demonstrate the relationship between thyroid function and taking these drugs. Future studies and investigations can be conducted on various animal models. Knowledge of the site of drug interaction and the physiologic features of the thyroid should enable the clinician to anticipate changes that may occur in thyroid homeostasis. Being aware of drugs that raise the risk of thyroid abnormalities would help in monitoring those patients at high risk and would lead to early diagnosis and treatment. Potential effects of these drugs on the results of thyroid function must always be considered in decisions regarding patient care. Much further work will be required to confirm these theories. The relationship between the thyroid and some psychoactive drugs is generally unknown, further studies are required in this field. A better understanding of the influence of thyroid status on antidepressant treatments could help to improve their efficacy.
Acknowledgements
We appreciate Ass. Prof. Dr. Yousef Rasmi for technical assistance.
Conflict of interest: The authors have no conflict of interest.
References
1. Baumeister A. The chlorpromazine enigma. J Hist Neurosci 2013;22:14–29.10.1080/0964704X.2012.664087Search in Google Scholar
2. Khalil RB, Richa S. Thyroid adverse effects of psychotropic drugs: a review. Clin Neuropharmacol 2011;34:248–55.10.1097/WNF.0b013e31823429a7Search in Google Scholar
3. Fraser AD. Use and abuse of the benzodiazepines. Ther Drug Monit 1998;20:481–9.10.1097/00007691-199810000-00007Search in Google Scholar
4. Lim CF, Loidl NM, Kennedy JA, Topliss DJ, Stokigt JR. Effect of loop diuretics and nonsteroidal antiinflammatory drugs on thyrotropin release by rat anterior pituitary cells in vitro. Metabolism 1995;44:1008–12.10.1016/0026-0495(95)90097-7Search in Google Scholar
5. Zevenbergen C, Korevaar TI, Schuette A, Peeters RP, Medici M, Visser TJ, et al. Association of antiepileptic drug usage, trace elements and thyroid hormone status. Eur J Endocrinol 2016;174:425–32.10.1530/EJE-15-1081Search in Google Scholar PubMed
6. Sauvage M, Marquet P, Rousseau A, Raby C, Buxeraud J, Lachâtre G. Relationship between psychotropic drugs and thyroid function: a review. Toxicol Appl Pharmacol 1998;149:127–35.10.1006/taap.1998.8367Search in Google Scholar PubMed
7. Bunevicius R, Vesta S, Arthur JP. Thyroid axis function after in-patient treatment of acute psychosis with antipsychotics: a naturalistic study. BMC Psychiatry 2014;14:279.10.1186/s12888-014-0279-7Search in Google Scholar PubMed PubMed Central
8. Evans PJ, Woodhead JS, Weeks I, Scanlon MF. Circulating TSH levels measured with an immunochemiluminometric assay in patients taking drugs interfering with biochemical thyroid status. Clin Endocrinol (Oxf) 1987;26:717–21.10.1111/j.1365-2265.1987.tb00831.xSearch in Google Scholar PubMed
9. Correll CU, Carlson HE. Endocrine and metabolic adverse effects of psychotropic medications in children and adolescents. J Am Acad Child Adolesc Psychiatry 2006;45:771–91.10.1097/01.chi.0000220851.94392.30Search in Google Scholar PubMed
10. Ulusu NN, Yılmaz G, Erbayraktar Z, Evlice A, Genç M, Aras S, et al. Comparative study on thyroid function in Alzheimer`s disease: results from a turkish multi-centre study. Journal of J Neurol Sci Turk 2015;32:335–47.Search in Google Scholar
11. Lambert CG, Mazurie AJ, Lauve NR, Hurwitz NG, Young SS, Obenchain RL, et al. Hypothyroidism risk compared among nine common bipolar disorder therapies in a large US cohort. Bipolar Disord 2016;18:247–60.10.1111/bdi.12391Search in Google Scholar PubMed PubMed Central
12. O’Brien CP. Benzodiazepine use, abuse, and dependence. J Clin Psychiatry 2005;66:28–33.Search in Google Scholar
13. Wolf B, Griffiths RR. Physical dependence on benzodiazepines: differences within the class. Drug Alcohol Depend 1991;29: 153–6.10.1016/0376-8716(91)90044-YSearch in Google Scholar
14. Chouinard G. Issues in the clinical use of benzodiazepines: potency, withdrawal, and rebound. J Clin Psychiatry 2004;65:7–12.Search in Google Scholar
15. Ottenweller JE, Tapp WN, Natelson BH. Effects of chronic alprazolam treatment on plasma concentrations of glucocorticoids, thyroid hormones, and testosterone in cardiomyopathic hamsters. Psychopharmacology 1989;98:369–71.10.1007/BF00451689Search in Google Scholar
16. Górska A, Marszałł M, Sloderbach A. The neurotoxicity of pyridinium metabolites of haloperidol. Postepy Hig Med Dosw 2015;19:1169–1175.10.5604/17322693.1175009Search in Google Scholar
17. Kudo S, Ishizaki T. Pharmacokinetics of haloperidol: an update. Clin Pharmacokinet 1999;37:435–56.10.2165/00003088-199937060-00001Search in Google Scholar
18. Andreassen OA, Aamo TO, Jorgensen HA. Inhibition by memantine of the development of persistent oral dyskinesias induced by long-term haloperidol treatment of rats. Br J Pharmacol 1996;119:751–7.10.1111/j.1476-5381.1996.tb15736.xSearch in Google Scholar
19. Markianos M, Hatzimanolis J, Stefanis C. Prolactin and TSH responses to TRH and to haloperidol in schizophrenic patients before and after treatment. Eur Neuropsychopharmacol 1994;4:513–6.10.1016/0924-977X(94)90300-XSearch in Google Scholar
20. Hodgson NA, Gitlin LN, Winter L, Czekanski K. Undiagnosed illness and neuropsychiatric behaviors in community residing older adults with dementia. Alzheimer Dis Assoc Disord 2011;25:109–15.10.1097/WAD.0b013e3181f8520aSearch in Google Scholar PubMed PubMed Central
21. Ulusu NN. Glucose-6-phosphate dehydrogenase deficiency and Alzheimer’s disease: Partners in crime. The hypothesis. Med Hypotheses 2015;85:219–23.10.1016/j.mehy.2015.05.006Search in Google Scholar PubMed
22. Torrigiani G, Deborah D, Roitt IM. Serum thyroglobulin levels in healthy subjects and in patients with thyroid disease. J Clin Endocrinol Metab 1969;29:305–14.10.1210/jcem-29-3-305Search in Google Scholar PubMed
23. Ulusu NN. Curious Cases of the Enzymes. J Med Biochem 2015;34:271–81.10.2478/jomb-2014-0045Search in Google Scholar PubMed PubMed Central
24. National Center for Biotechnology Information. PubChem Compound Database; CID=2118, https://pubchem.ncbi.nlm.nih.gov/compound/2118 (accessed Nov. 15, 2015).Search in Google Scholar
25. National Center for Biotechnology Information. PubChem Compound Database; CID=3559, https://pubchem.ncbi.nlm.nih.gov/compound/2118 (accessed Apr. 26, 2016).Search in Google Scholar
26. Lipska BK, Khaing ZZ, Weickert CS, Weinberger DR. BDNF mRNA expression in rat hippocampus and prefrontal cortex: effects of neonatal ventral hippocampal damage and antipsychotic drugs. Eur J Neurosci 2001;14:135–44.10.1046/j.1460-9568.2001.01633.xSearch in Google Scholar PubMed
27. Kapur S, Wadenberg ML, Remington G. Are animal studies of antipsychotics appropriately dosed? Lessons from the bedside to the bench. Can J Psychiatry 2000;45:241–6.10.1177/070674370004500302Search in Google Scholar PubMed
28. Halim ND, Weickert CS, McClintock BW, Weinberger DR, Lipska BK. Effects of chronic haloperidol and clozapine treatment on neurogenesis in the adult rat hippocampus. Neuropsychopharmacology 2004;29:1063–9.10.1038/sj.npp.1300422Search in Google Scholar PubMed
29. Elmesallamy GE, Abass MA, Ahmed NA, Atta AH. Differential effects of alprazolam and clonazepam on the immune system and blood vessels of non-stressed and stressed adult male albino rats. Interdiscip Toxicol 2011;4:132–43.10.2478/v10102-011-0021-ySearch in Google Scholar PubMed PubMed Central
30. Spence AL, Guerin GF, Goeders NE. Differential modulation of the discriminative stimulus effects of methamphetamine and cocaine by alprazolam and oxazepam in male and female rats. Neuropharmacology 2016;102:146–57.10.1016/j.neuropharm.2015.10.041Search in Google Scholar PubMed
31. Liu ZW, Masterson L, Fish B, Jani P, Chatterjee K. Thyroid surgery for Graves’ disease and Graves’ ophthalmopathy. Cochrane Database Syst Rev 2015;25:CD010576.10.1002/14651858.CD010576.pub2Search in Google Scholar PubMed
32. Sabeen S, Chou C, Holroyd S. Abnormal thyroid stimulating hormone (TSH) in psychiatric long-term care patients. Arch Gerontol Geriatr 2010;51:6–8.10.1016/j.archger.2009.06.002Search in Google Scholar PubMed
33. Engum A, Bjoro T, Mykletun A, Dahl AA. An association between depression, anxiety and thyroid function–a clinical fact or an artefact? Acta Psychiatr Scand 2002;106:27–34.10.1034/j.1600-0447.2002.01250.xSearch in Google Scholar PubMed
34. Kibirige D, Luzinda K, Ssekitoleko R. Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res 2013;6:2–5.10.1186/1756-6614-6-3Search in Google Scholar PubMed PubMed Central
35. Borison RL. Recent advances in the pharmacotherapy of schizophrenia. Harv Rev Psychiatry 1997;4:255–71.10.3109/10673229709030552Search in Google Scholar PubMed
36. Bunevicius R, Steibliene V, Prange AJ. Thyroid axis function after in-patient treatment of acute psychosis with antipsychotics: a naturalistic study. BMC Psychiatry 2014;14:2–9.10.1186/s12888-014-0279-7Search in Google Scholar
37. Kahilogullari AK, Orsel S, Karadag H, Akdemir A, Hatiloglu U. The effectiveness of thyroid function tests screening in psychiatric in-patients. Bull Clin Psychopharm 2010;20:234–9.10.1080/10177833.2010.11790664Search in Google Scholar
38. Gitlin M, Altshuler L, Frye MA, Suri R. Peripheral thyroid hormones and response to selective serotonin reuptake inhibitors. Jf Psychiatry Neurosci 2004;29:383.Search in Google Scholar
39. Davies PH, Franklyn JA. The effects of drugs on tests of thyroid function. Eur J Clin Pharmacol 1991;40:439–51.10.1007/BF00315221Search in Google Scholar
40. Lindsey PL. Psychotropic medication use among older adults: what all nurses need to know. J Gerontol Nurs 2009;35:28–38.10.3928/00989134-20090731-01Search in Google Scholar
41. Sauvage MF, Marqquet P, Rousseau A, Raby C, Buxeraud J, Lachatre G. Relationship between psychotropic drugs and thyroid function: a review. Toxicol Appl Pharmacol 1998;149:127–35.10.1006/taap.1998.8367Search in Google Scholar
42. Lazarus JH. Lithium and thyroid. Best Pract Res. Clin Endocrinol Metab 2009;23:723–33.10.1016/j.beem.2009.06.002Search in Google Scholar
43. Langlois MC, Beaudry G, Zekki H, Rouillard C, Levesque D. Impact of antipsychotic drug administration on the expression of nuclear receptors in the neocortex and striatum of the rat brain. Neuroscience 2001;106:117–28.10.1016/S0306-4522(01)00248-2Search in Google Scholar
44. Baumgartner A, Pietzcker A, Gaebel W. The hypothalamic–pituitary–thyroid axis in patients with schizophrenia. Schizophr Res 2000;44:233–43.10.1016/S0920-9964(99)00187-5Search in Google Scholar
45. Emul MA, Sakalli TC, Erol TC, Ertan T. Thyrotoxic psychosis in an elderly woman and haloperidol use: a case report. Psychogeriatrics 2013;13:49–51.10.1111/j.1479-8301.2012.00404.xSearch in Google Scholar PubMed
©2018 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Frontmatter
- Research Articles
- The use of six sigma methodology to evaluate the analytical performances of clinical chemistry analyzers
- Evaluation of clinical chemistry tests in emergency laboratory by sigma metrics
- Neutrophil gelatinase associated lipocalin, an early biomarker for diagnosis of acute kidney injury after percutaneous coronary intervention
- Increased serum levels of spectrin degradation products in patients with schizophrenia
- Concentrations of circulating adiponectin and adipocyte-fatty acid binding protein in patients with three-vessel coronary artery disease: a comparison with coronary lesion complexity as characterized by syntax score
- Effects of aerobic plus explosive power exercises on bone remodeling and bone mineral density in young men
- Evaluation of serum 25-hidroxy vitamin D and zinc levels in asthmatic patients
- Effects of alprazolam and haloperidol on thyroglobulin, antithyroglobulin, anti thyroid peroxidase and TSH in Rat
- Evaluation of laboratory parameters in the diagnosis of acute appendicitis
- Assessment of macroprolactinemia inpatients with prolactinoma
- Evaluation of vascular endothelial growth factor levels in rheumatoid arthritis patients, with and without joint swelling; a comparison with erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor and anti-cyclic citruillnated protein
- Fibroblast growth factor-23 concentrations in polycystic ovary syndrome
- Opinion Papers
- Evaluation of H-800/FUS-100 automatic urine analyzer performance
- Determining knowledge of the nursing students about biochemistry laboratory samples
- Letter to the Editor
- Response to Letter to the Editor, “Some errors in the measurement of neutrophil-to-lymphocyte ratio”
- Short Communication
- How to decrease the rejection rates: reasons of sample rejection and solutions
Articles in the same Issue
- Frontmatter
- Research Articles
- The use of six sigma methodology to evaluate the analytical performances of clinical chemistry analyzers
- Evaluation of clinical chemistry tests in emergency laboratory by sigma metrics
- Neutrophil gelatinase associated lipocalin, an early biomarker for diagnosis of acute kidney injury after percutaneous coronary intervention
- Increased serum levels of spectrin degradation products in patients with schizophrenia
- Concentrations of circulating adiponectin and adipocyte-fatty acid binding protein in patients with three-vessel coronary artery disease: a comparison with coronary lesion complexity as characterized by syntax score
- Effects of aerobic plus explosive power exercises on bone remodeling and bone mineral density in young men
- Evaluation of serum 25-hidroxy vitamin D and zinc levels in asthmatic patients
- Effects of alprazolam and haloperidol on thyroglobulin, antithyroglobulin, anti thyroid peroxidase and TSH in Rat
- Evaluation of laboratory parameters in the diagnosis of acute appendicitis
- Assessment of macroprolactinemia inpatients with prolactinoma
- Evaluation of vascular endothelial growth factor levels in rheumatoid arthritis patients, with and without joint swelling; a comparison with erythrocyte sedimentation rate, C-reactive protein, rheumatoid factor and anti-cyclic citruillnated protein
- Fibroblast growth factor-23 concentrations in polycystic ovary syndrome
- Opinion Papers
- Evaluation of H-800/FUS-100 automatic urine analyzer performance
- Determining knowledge of the nursing students about biochemistry laboratory samples
- Letter to the Editor
- Response to Letter to the Editor, “Some errors in the measurement of neutrophil-to-lymphocyte ratio”
- Short Communication
- How to decrease the rejection rates: reasons of sample rejection and solutions

