The relationship between patient factors and the refusal of analgesics in adult Emergency Department patients with extremity injuries, a case-control study
-
Milan L. Ridderikhof
, Donica V. Lodder
Abstract
Background and aims
Previous studies have described the phenomenon of oligo-analgesia in Emergency Department patients with traumatic injuries, despite the high prevalence of pain among these patients. Besides aspects related to health care staff, patient related factors might also play a role in suboptimal pain treatment, however evidence is scarce. Therefore, the objective of the current study was to evaluate patient related factors in adult patients refusing offered analgesics during an Emergency Department presentation with extremity injuries.
Methods
This was a case control study in the Emergency Department of a level 1 Trauma Centre. Cases were defined as adult patients with an extremity injury who declined analgesia, when offered. They were matched to controls from the same population, who accepted analgesics, in a 1:2 ratio using gender as matching variable. Primary outcome was difference in NRS pain score. Secondary outcomes were the relationship between categorical severity of pain scores and refusal of analgesics, exploration of independent predictors of analgesia refusal utilizing multivariate logistic regression and the evaluation of eight beliefs among patients who refuse analgesics.
Results
Between August 1st and 31st 2016, a total of 253 patients were eligible for inclusion of whom 55 declined analgesic treatment. They were included as cases and matched to 110 controls. Difference in median NRS pain score was significant between the groups: 5.0 (IQR 3.0–8.0) vs. 8.0 (IQR 6.0–9.0), respectively (p < 0.01). Nearly 20% of patients with severe pain declined analgesics, compared to 41% with moderate and 69% with mild pain (p < 0.01). The NRS pain score was the only independent predictor of refusal of analgesic treatment with a mean Odds Ratio of 0.67 (95%-CI 0.54–0.83). Most common patients’ beliefs were that pain medication should be used in extreme pain only, fear of decreasing the doctor’s ability to judge the injury and fear of addiction to analgesics.
Conclusions
Pain severity is the single independent predictor of refusal of analgesia, however the following patient beliefs are important as well: pain medication should be used in extreme pain only; fear of decreasing the doctor’s ability to judge the injury and the fear of becoming addicted to pain medication.
Implications
In case patients refuse offered analgesics, the health care provider should actively address patient beliefs that might exist and lead to suboptimal pain treatment.
1 Introduction
Patients with extremity injuries are frequently treated in the Emergency Department. Examples of these injuries are fractures, contusions or strains and sprains. As these injuries are often painful, treatment usually consists of pain treatment with orally or intravenously administered analgesics, besides injury-specific treatment, such as immobilization or elevation. Although the prevalence of pain in patients with traumatic injuries in the Emergency Department is high, previous studies have consistently shown that pain is treated inadequately [1], [2], [3]. Several factors could contribute to this phenomenon of “oligo-analgesia” in the Emergency Department and have previously been described among health care staff [4]. Lack of assessment or underestimation of pain severity play a role, as pain scores are used infrequently and health care staff tends to underestimate pain severity in general [2], [3], [5], [6]. Moreover, concerns about masking occult injury and fear of side effects related to administration of analgesics might explain inappropriate use of pain medication [7]. However, besides these aspects, patient related factors might be as important as well, as patients might decline analgesics for various reasons. For instance, more than 10% of patients with long bone fractures declined pain medication, despite having pain [8]. Reasons for declining analgesics were not reported in this study. The authors of a 2008 study found that nearly 50% in a cohort of Emergency Department patients with traumatic as well as non-traumatic painful conditions refused analgesics [9]. As expected, patients wanting analgesics had higher pain scores than patients who refused analgesics and the main reason not to want analgesics was that pain was considered tolerable. Other reasons patients reported were that they had already taken analgesics at home and that they wanted to stay alert. Additional reasoning have been published elsewhere and included the belief that analgesics should be given only when pain was unbearable [5]. Moreover, in another study in 203 Emergency Department patients presenting with painful injuries, fear of addiction was the most reported reason for analgesic refusal [10].
As mentioned, pain severity seems of importance in the patient’s decision whether to accept or decline analgesics, however there are conflicting results as another Emergency Department study found no relationship between pain severity and desire for analgesia [11], [12]. Because of these conflicting results and the fact that previous studies mainly evaluated mixed study populations with both traumatic and non-traumatic conditions, the current study was undertaken. The objective was to evaluate differences between patients presenting with extremity injuries who accepted and patients who refused analgesics. Moreover, patient related factors were evaluated in patients refusing analgesics. The rationale of this study was that knowledge of these factors is potentially useful in optimizing future Emergency Department pain treatment and make steps towards patient centered pain treatment instead of protocol centered pain treatment.
2 Methods
2.1 Study design
The current study was a case-control study. Approval of the Institutional Review Board (IRB) was obtained and a waiver was supplied as the questions patients were asked were not regarded as additional intervention (number W16_21316#249).
2.2 Study setting and population
The study was conducted in the Emergency Department of a Level one trauma centre. During the recruitment period, trained research assistants were present in the Emergency Department from 12 to 8 pm from Monday to Friday. Patients who presented during these hours were considered eligible and approached for inclusion in the study in case they presented with an acute injury of an extremity, that occurred within 48 h prior to presentation; were at least 18 years or older and declined analgesic treatment, which is offered to all patients presenting to the Emergency Department. An acute extremity injury was defined as (suspicion of) a fracture, sprain, strain or a wound on an extremity. Exclusion criteria were arrival by ambulance; cognitive impairment; self-inflicted injury and intoxication.
Control patients were randomly selected from the same Emergency Department population from the same study period and were required to accept analgesic treatment for their acute extremity injury. Cases were matched with controls using a control-to-case ratio of 2:1 and were matched on gender, as this factor has previously been correlated with higher pain scores [13], [14], [15].
2.3 Study protocol
During presentation to the Emergency Department, standard practice dictates that the triage nurse evaluates Numerical Rating Scale (NRS) pain scores and offers pain medication in case pain is present. A nurse-initiated pain management protocol allows triage nurses to administer paracetamol, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and/or fentanyl autonomously, without consulting a physician and analgesic choices are based on pain severity scores [3]. During the recruitment period, the research assistant approached patients who declined analgesic treatment after the triage nurse recorded the NRS pain score and offered analgesia. Patients were asked to fill in a standard case report form in which all data were collected anonymously. Data included the Barriers questionnaire, which has been validated previously in chronic pain research and consists of eight statements with six-point Likert scales whereby answers range from “do not agree at all” to “agree very much” [16]. Besides the questions from this questionnaire, pain scores were recorded utilizing the 11-point NRS, in which zero means no pain and ten is the worst pain imaginable. This pain score has been validated in the Emergency Department previously [17]. Moreover, injury localization (upper or lower extremity), trauma mechanism (sharp or blunt), diagnosis at discharge and time between injury and presentation to the Emergency Department were recorded as well.
2.4 Outcomes
The primary study outcome was the difference in initial NRS pain scores between patients who declined analgesic treatment (cases), compared to patients who accepted analgesic treatment (controls).
Secondary outcomes included the relationship between categories of pain severity and refusal of analgesics and exploration of independent predictors of analgesia refusal utilizing multivariate logistic regression. Additionally, factors that could independently predict the decision to refuse analgesic treatment were evaluated in patients declining pain medication.
2.5 Statistical analysis
Previously, a standard deviation in NRS pain score of 2.06 NRS points was found in this study population (unpublished data). Using this standard deviation and a 0.05 two-sided significance level, a sample size of 54 patients in each group would have 90% power to detect a minimally clinically relevant difference in NRS pain scores of 1.3 NRS points. As the study was designed as a case-control study with a 1:2 matching ratio, the control group was twice as large. Utilizing this group ratio of 1:2, the study was able to detect a difference of 0.54 NRS points between the two groups. It was expected that during an inclusion period of 4 weeks enough patients would have been recruited.
Collected data were presented as absolute values with proportions, in case of descriptive parameters, such as the Barriers questionnaire. Continuous data were reported as mean values with a 95%-Confidence Interval (95%-CI) or median values with an interquartile range (IQR), depending on normality of the data. This was tested by visual inspection of the histogram of all NRS pain scores. Categorical data were analyzed using the Chi Square test or the Fisher Exact Test and numerical values with a normal distribution were evaluated using the Students t-test. The Mann-Whitney U test was used for analysis of numerical values without a normal distribution. In order to identify independent predictors for refusal of analgesic treatment, a multivariate logistic regression model was designed utilizing all available variables. For this purpose, univariable preselection was performed initially. Subsequently, best performing parameters with a p-value below 0.2 were used in a multivariate logistic regression model. In case of categorical variables, the largest category was used as the reference category. In order to prevent multicollinearity, two separate models were built for the potential linearly related parameters trauma mechanism and diagnosis at discharge. For all statistical analyses, a p-value of 0.05 indicated statistical significance. Data were analyzed using SPSS version 24 (Chicago, IL, USA).
3 Results
3.1 Study characteristics
During the recruitment period of 4 weeks between August 1st and September 1st 2016, a total of 253 patients were potentially eligible for enrolment in the study. A total of 55 patients declined analgesic treatment at triage and were matched to 110 patients who accepted analgesic treatment (Fig. 1).
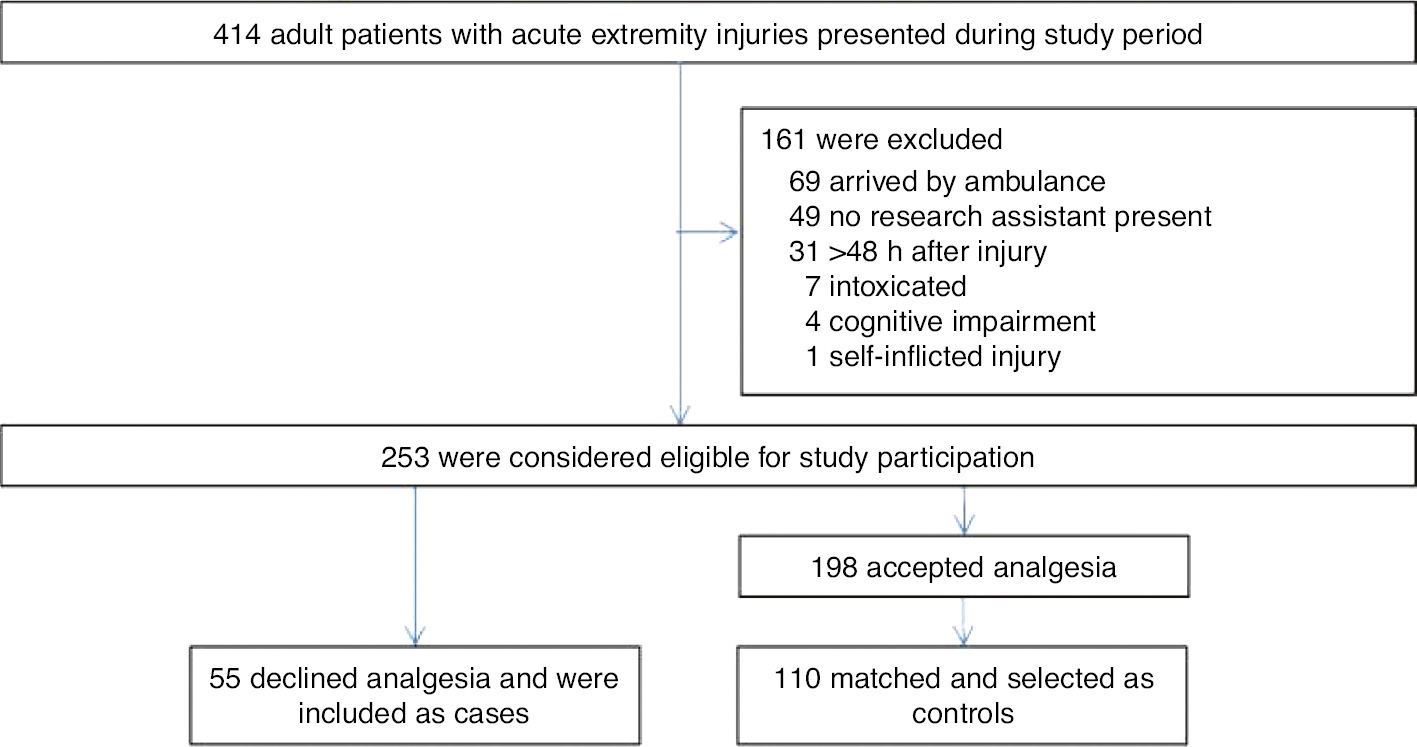
Patient flow chart. A total of 414 patients with acute traumatic extremity injuries presented to the Emergency Department during the study period, of which 253 were eligible for inclusion in the study. From this population 55 cases and 110 controls were selected.
Baseline characteristics are shown in Table 1. Most patients were male with an injury of the upper extremity after sustaining blunt direct trauma. There were no statistical differences between the cases and the groups, except for the diagnosis at discharge, as significantly more patients who presented with a wound refused pain medication, compared to patients presenting with fractures or presenting with strains or sprains.
Baseline parameters.
| Parameter | Cases (N=55) | Controls (N=110) | Total (N=165) | p-Value |
|---|---|---|---|---|
| Male sex (%) | 39 (70.9) | 78 (70.9) | 117 (70.9) | >0.99 |
| Median age in years (IQR) | 43.6 (30.2–54.6) | 38.9 (26.4–51.4) | 39.5 (27.1–52.7) | 0.29 |
| Injured extremity (%) | 0.83 | |||
| Upper extremity | 29 (52.7) | 60 (54.5) | 89 (53.9) | |
| Lower extremity | 26 (47.3) | 50 (45.5) | 76 (46.1) | |
| Trauma mechanisma (%) | 0.17 | |||
| Direct, blunt | 26 (47.3) | 66 (60.0) | 92 (55.8) | |
| Direct, sharp | 12 (21.8) | 13 (11.8) | 25 (15.2) | |
| Indirect | 17 (30.9) | 31 (28.2) | 48 (29.1) | |
| Time to presentationb (%) | 0.72 | |||
| <6 h | 29 (69.0) | 67 (65.7) | 96 (66.7) | |
| 6–12 h | 3 (7.1) | 12 (11.8) | 15 (10.4) | |
| 12–18 h | 1 (2.4) | 6 (5.9) | 7 (4.9) | |
| 18–24 h | 3 (7.1) | 4 (3.9) | 7 (4.9) | |
| 24–48 h | 6 (14.3) | 13 (12.7) | 19 (13.2) | |
| Diagnosis at discharge (%) | <0.01 | |||
| Sprain or strain | 18 (32.7) | 55 (50.0) | 73 (44.2) | |
| Fracture | 11 (20.0) | 36 (32.7) | 47 (28.5) | |
| Wound | 26 (47.3) | 19 (17.3) | 45 (27.3) |
-
aIndirect trauma was defined as twisting or rotating trauma mechanism, as well as an inversion of a joint. A direct trauma required a direct force to be applied to the body. bIn a total of 21 patients data regarding time to presentation was missing (13 in the cases group and 8 in the control group). IQR=interquartile range; NRS=Numerical Rating Scale.
3.2 Outcomes
NRS pain scores were not distributed normally, as the histogram revealed a distribution that was skewed to the right. The median NRS pain score in the group of patients who declined analgesic treatment was 5.0 (IQR 3.0–8.0) and 8.0 (IQR 6.0–9.0) in the control group who accepted analgesia. The difference in NRS scores between these groups was statistically significant (p<0.01) and the distribution of median NRS pain scores of both groups is shown in Fig. 2.
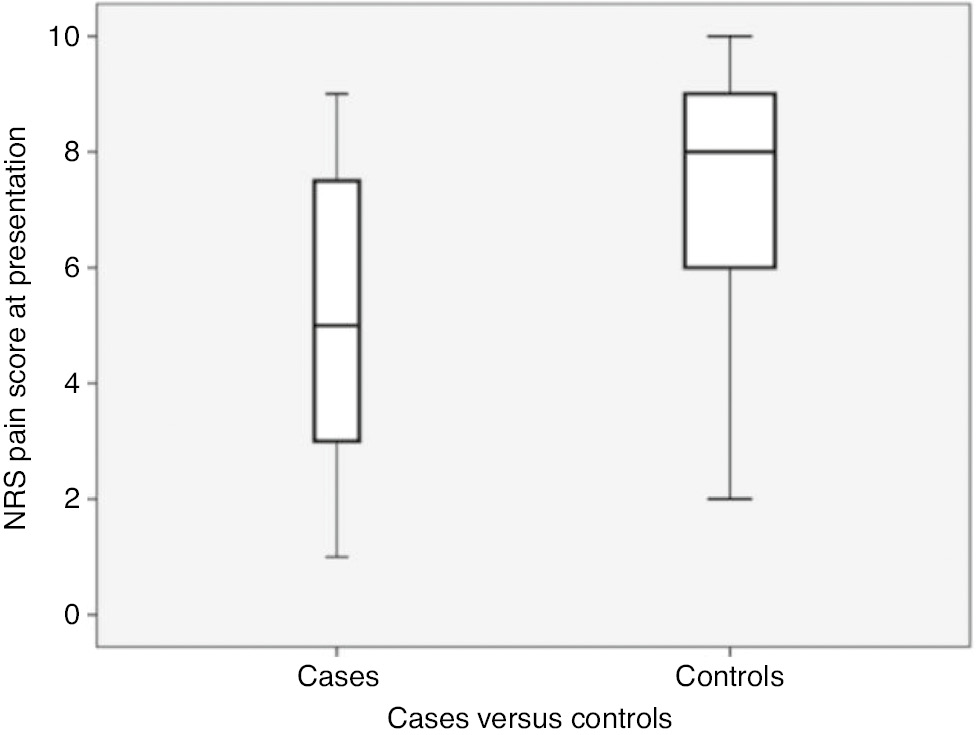
NRS pain scores of cases and controls. Box plots of patients declining analgesics (cases) and patients accepting analgesics (controls), showing distribution of NRS pain scores. The box represents the median NRS value with its 1st and 3rd quartile and the whiskers show the minimum and maximum NRS value in each group. NRS, Numerical Rating Scale.
Of all patients, 29 (17.6%) reported minor pain (NRS pain score 1–3), 39 (23.6%) reported moderate pain (NRS 4–6) and 97 patients (58.8%) reported severe pain (NRS pain score 7 or higher).
Nineteen patients (19.6%) with severe pain, 16 patients (41%) with moderate pain and 20 patients (69.0%) with minor pain did not desire analgesic treatment when offered (p<0.01).
Tables 2 and 3 show the results of the logistic regression models in which refusal of analgesia is utilized as binary outcome. Trauma mechanism, diagnosis at discharge and NRS pain scores entered the multivariate models as independent variables after univariable preselection.
Univariable logistic regression model.
| Parameter | OR (95%-CI) | p-Value |
|---|---|---|
| Age | 1.01 (0.99–1.03) | 0.439 |
| Injury localization | 1.08 (0.56–2.06) | 0.83 |
| Trauma mechanisma | 0.17 | |
| Indirect | 1.39 (0.66–2.93) | |
| Direct, sharp | 2.34 (0.95–5.80) | |
| NRS pain score | 0.67 (0.57–0.78) | <0.01 |
| Time to presentationb | 0.70 | |
| 6–12 h | 0.58 (0.15–2.20) | |
| 12–18 h | 0.39 (0.044–3.34) | |
| 18–24 h | 1.73 (0.36–8.26) | |
| 24–48 h | 1.07 (0.37–3.08) | |
| Discharge diagnosisc | <0.01 | |
| Wound | 4.18 (1.89–9.27) | |
| Fracture | 0.93 (0.40–2.21) |
-
All available variables were entered in a univariable preselection model. aAs “direct blunt trauma” was the largest category, this was used as the reference category. bAs “within 6 h” was the largest category, this was used as the reference category. cAs “strains and sprains” was the largest category, this was used as the reference category. OR=odds ratio; 95%-CI=95%-confidence interval; NRS=Numerical Rating Scale.
Multivariable logistic regression model.
| Parameter | OR (95%-CI) | p-Value |
|---|---|---|
| Trauma mechanisma | 0.54 | |
| Indirect | 1.30 (0.57–2.96) | |
| Direct, sharp | 0.67 (0.22–2.03) | |
| NRS pain scoreb | 0.64 (0.54–0.77) | <0.01 |
| Discharge diagnosisc | 0.29 | |
| Wound | 2.04 (0.83–5.03) | |
| Fracture | 1.12 (0.45–2.76) | |
| NRS pain scoreb | 0.70 (0.59–0.83) | <0.01 |
-
The best performing predicting factors from the univariable regression analysis were entered into a multivariate logistic regression model, in case the p-value was 0.2 or lower. aAs “direct blunt trauma” was the largest category, this was used as the reference category. bIn order to prevent multicollinearity, NRS pain score was analyzed in one model with trauma mechanism and in another model with discharge diagnosis. cAs “strains and sprains” was the largest category, this was used as the reference category. OR=odds ratio; 95%-CI=95%-confidence interval; NRS=Numerical Rating Scale.
In order to prevent multicollinearity, both trauma mechanism and discharge diagnosis were entered into separate models, which were corrected for NRS pain scores. Both indirect and direct sharp trauma mechanism as well as wound and fracture as discharge diagnosis did not significantly or independently predict refusal of analgesics. In both models, NRS pain score at presentation was a significant predictor of refusal of analgesics, as the Odds Ratios were 0.64 (95%-CI 0.54–0.77; p<0.01) and 0.70 (95%-CI 0.59–0.83; p<0.01), respectively. This means that for every increase in NRS by one point, the risk of refusal of pain medication decreases with approximately one third.
The results of the Likert scales of the eight-item Barriers questionnaire are shown in Fig. 3. The three statements patients agreed most with, were: “pain medication should only be used in extreme pain” (45.5% very much agreed and 25.5% agreed); “pain medication decreases the doctor’s ability to appropriately judge the injury” (20% very much agreed and 29.1% agreed) and “people easily get addicted to pain medication” (21.8% very much agreed and 21.8% much agreed). However, regarding the latter statement, a total of 27.3% did not agree at all.
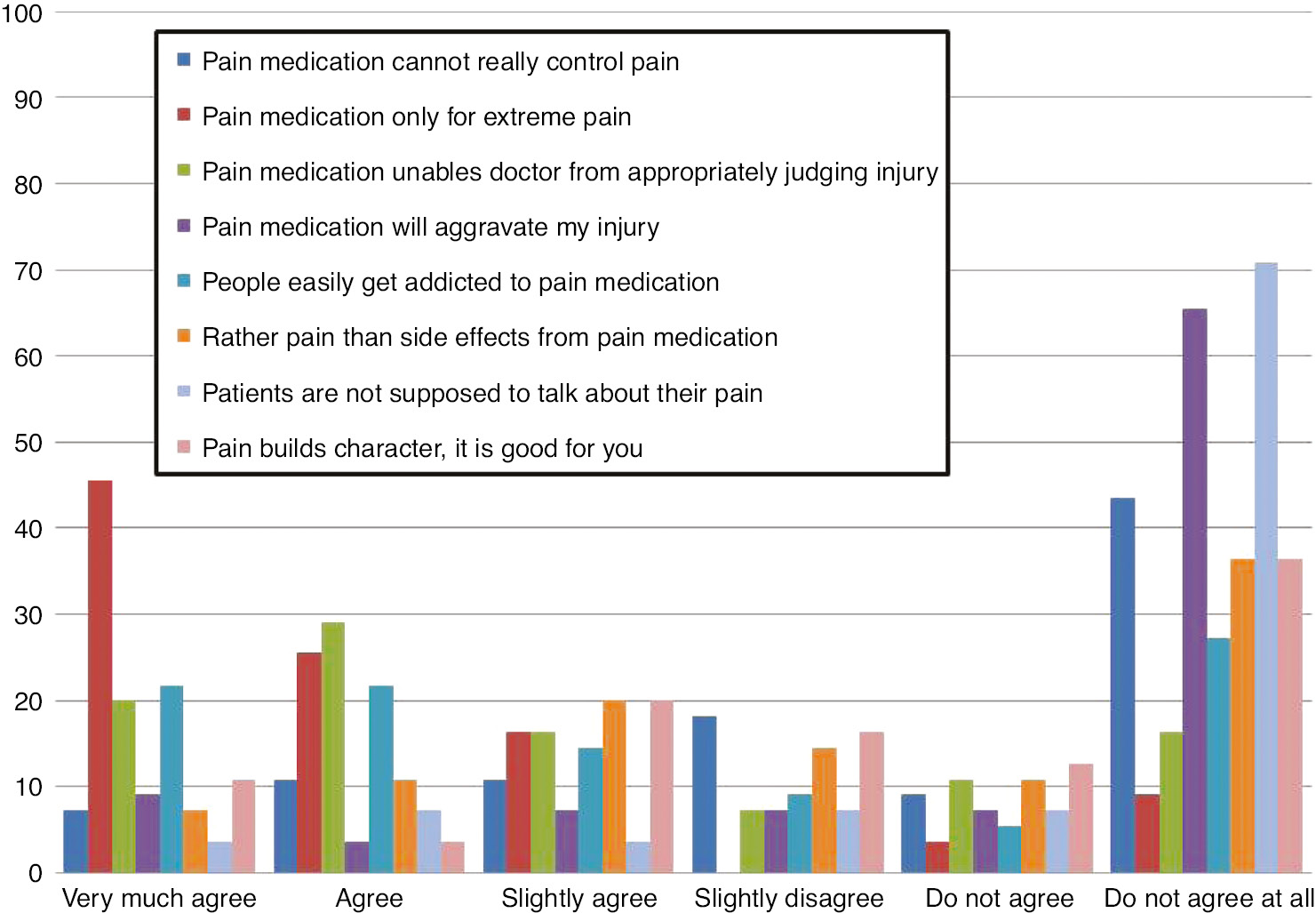
Results of the Barriers Questionnaire. The 6-point Likert scale answers to the eight items of the Barriers questionnaire. On the x-axis results are shown in percentages.
The three statements patients did not agree with most profoundly were: “patients are not supposed to talk about their pain” (70.9% do not agree at all and 7.3% do not agree); “pain medication will aggravate my injury” (65.5% do not agree at all and 10.9% do not agree) and “pain medication cannot really control pain” (43.6% do not agree at all and 9.1% do not agree).
4 Discussion
In the current study we evaluated reasons why adult patients presenting to the Emergency Department with extremity injuries decline analgesic treatment. The results show that the lower the median NRS pain score, the more likely it is that patients refuse analgesic treatment. In other words, pain scores were significantly higher in patients who accepted analgesic treatment compared to patients who declined this. The logistic regression model supported this by showing that the initial NRS pain score was inversely related to refusal of pain medication with a mean Odds Ratio of 0.67. In line with these findings most patients who declined analgesia agreed that pain medication should be reserved for extreme pain only.
The authors of an observational, prospective, multicenter study in the United States and Canada in 842 patients with acute pain due to various traumatic and non-traumatic causes reported that 30% of all patients did not want analgesic treatment [12]. Of these, 49% of patients with moderate pain and 16% of patients with severe pain did not desire analgesics. These numbers are comparable to our results, as we found that 19.6% of patients with severe pain and 41% of patients with moderate pain refused analgesics.
It seems that our patients did not find it difficult to talk about pain, as they most profoundly disagreed with the statement that “patients should not talk about their pain”. This is in contradiction to the results of a previous survey performed among New Zealand Emergency Department nurses [18]. These authors identified reluctance of patients to report pain as the most important patient-related barrier to optimal pain treatment. These contrasting results emphasize the importance of communication and explicitly asking patients whether this might play a role in declining analgesia.
A significant number of respondents in the same survey perceived patients’ reluctance to take opioids as barrier as well. It was not clear whether fear of adverse events or fear of dependence played a role. The results from our questionnaire did not explicitly reveal this. Although a total of 40% of our study population agreed or agreed very much with the statement of addiction, 27.3% did not agree at all. Additionally, 36.4% of our patients did not agree with the statement to rather have pain than side effects. The same was found by Singer et al. who reported that a only a minority of 7% of patients who declined analgesic treatment gave as reason that they did not want to become groggy and wanted to stay alert [9].
The same authors reported that the most common patient-related factor in their study was that pain was tolerable. Stalnikowicz et al. described that 66% of all patients who were interviewed regarding misconceptions about pain management agreed with the statement that pain medication should only be used when pain was unbearable [5]. These findings match our study results as one of the three statements patients agreed with most, was that “pain medication should only be used in extreme pain”.
Besides this belief, nearly half of our patients agreed or agreed very much with the statement that pain medication would decrease the ability of the physician to judge the injury. This statement resembles the clinical myth that opioids should not be administered before assessment of a patient with abdominal pain, as this would “cloud” physician’s judgment. This myth was busted by the authors of a Cochrane review and therefore patients should be informed that administration of pain medication does not cloud judgment nor distracts the physician from the injury, as results of this review can probably extrapolated to patients with extremity injuries [19].
From our study results it becomes clear that regarding pain and pain medication, education of patients in the Emergency Department is of vital importance. We should inform them that analgesia is not only available for severe or extreme pain and that treating pain with pain medication does not mask symptoms or cloud judgment. As Ducharme concluded in 2013; in order to identify patient-related factors and beliefs, we have to start listening to our patients [20]. If patients do not want pain medication, we should ask them “why not?”
5 Limitations
We designed this study as a matched case-control study in order to isolate a cohort of patients who declined analgesia, a comparable group who did not decline analgesia and be able to correct for gender as this has been correlated with higher pain scores in previous research. There are several other factors we could also have matched for and by not doing so, we might have introduced bias. Examples are ethnicity and discharge diagnoses, as both might be important variables in analgesic treatment and pain severity.
Although an association between parameters can be found by choosing a case-control study design, a definitive cause-effect relationship cannot be determined [21].
We did not investigate whether patients received analgesics later on during their Emergency Department stay. It could have been that some patients changed their mind or only expressed their desire for pain medication to a physician. More importantly, pain medication already taken at home before Emergency Department presentation, were not accounted for.
In this study we used the Barriers questionnaire to evaluate pain experiences, beliefs and attitudes among patients with acute pain. It must be emphasized that this questionnaire has been validated in chronic pain patients and not in the acute setting. Moreover, as only patients who declined pain medication filled in this questionnaire, no comparison of motivations and beliefs between patients who accepted pain medication and patients who declined pain medication could be made.
The study population consisted of a convenience sample as the research assistant who collected patient data was not present in the Emergency Department all the time. Therefore, selection bias might have played a role, although it must be mentioned that only a minority of potentially eligible patients presenting to the Emergency Department and were not accounted for in retrospect. Moreover, patients were included in a level one trauma centre. Therefore, results might not be representative for all Emergency Departments.
Although the study was powered to detect a difference in NRS pain score between the two groups, the study population was relatively small and might not have been large enough to detect differences in other study variables.
6 Conclusions
In adult patients presenting to the Emergency Department with extremity injuries, pain severity is important in the decision to accept or decline analgesic treatment. However, common patient beliefs such as that analgesics should only be used in extreme pain, use of pain medication might prevent the doctor from appropriately judging the injury and fear of addiction, might also play a role in declining analgesic treatment. Therefore, in order to optimize pain treatment in the Emergency Department, these factors should actively be addressed by the emergency health care provider in case patients refuse analgesic treatment.
-
Authors’ statements
-
Research funding: Authors state no funding involved.
-
Conflict of interest: Authors state no conflict of interest.
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
-
Ethical approval: The research related to human use complies with all the relevant national regulations, institutional policies and was performed in accordance with the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board or equivalent committee.
References
[1] Berben SA, Meijs TH, van Dongen RT, van Vugt AB, Vloet LC, Mintjes-de Groot JJ, van Achterberg T. Pain prevalence and pain relief in trauma patients in the Accident & Emergency department. Injury 2008;39:578–85.10.1016/j.injury.2007.04.013Search in Google Scholar PubMed
[2] Brown JC, Klein EJ, Lewis CW, Johnston BD, Cummings P. Emergency department analgesia for fracture pain. Ann Emerg Med 2003;42:197–205.10.1067/mem.2003.275Search in Google Scholar PubMed
[3] Ridderikhof ML, Schyns FJ, Schep NW, Lirk P, Hollmann MW, Goslings JC. Emergency department pain management in adult patients with traumatic injuries before and after implementation of a nurse-initiated pain treatment protocol utilizing fentanyl for severe pain. J Emerg Med 2017;52:417–25.10.1016/j.jemermed.2016.07.015Search in Google Scholar PubMed
[4] Wilson JE, Pendleton JM. Oligoanalgesia in the emergency department. Am J Emerg Med 1989;7:620–3.10.1016/0735-6757(89)90286-6Search in Google Scholar PubMed
[5] Stalnikowicz R, Mahamid R, Kaspi S, Brezis M. Undertreatment of acute pain in the emergency department: a challenge. Int J Qual Health Care 2005;17:173–6.10.1093/intqhc/mzi022Search in Google Scholar PubMed
[6] Guru V, Dubinsky I. The patient vs. caregiver perception of acute pain in the emergency department. J Emerg Med 2000;18:7–12.10.1016/S0736-4679(99)00153-5Search in Google Scholar
[7] Lewis LM, Lasater LC, Brooks CB. Are emergency physicians too stingy with analgesics? South Med J 1994;87:7–9.10.1097/00007611-199401000-00002Search in Google Scholar PubMed
[8] Beel TL, Mitchiner JC, Frederiksen SM, McCormick J. Patient preferences regarding pain medication in the ED. Am J Emerg Med 2000;18:376–80.10.1053/ajem.2000.7313Search in Google Scholar PubMed
[9] Singer AJ, Garra G, Chohan JK, Dalmedo C, Thode Jr. HC. Triage pain scores and the desire for and use of analgesics. Ann Emerg Med 2008;52:689–95.10.1016/j.annemergmed.2008.04.017Search in Google Scholar PubMed
[10] Tanabe P, Buschmann M. A prospective study of ED pain management practices and the patient’s perspective. J Emerg Nurs 1999;25:171–7.10.1016/S0099-1767(99)70200-XSearch in Google Scholar
[11] Blumstein HA, Moore D. Visual analog pain scores do not define desire for analgesia in patients with acute pain. Acad Emerg Med 2003;10:211–4.10.1111/j.1553-2712.2003.tb01992.xSearch in Google Scholar PubMed
[12] Todd KH, Ducharme J, Choiniere M, Crandall CS, Fosnocht DE, Homel P, Tanabe P, PEMI Study Group. Pain in the emergency department: results of the pain and emergency medicine initiative (PEMI) multicenter study. J Pain 2007;8:460–6.10.1016/j.jpain.2006.12.005Search in Google Scholar PubMed
[13] Grimes DA, Schulz KF. Compared to what? Finding controls for case-control studies. Lancet 2005;365:1429–33.10.1016/S0140-6736(05)66379-9Search in Google Scholar PubMed
[14] Marco CA, Kanitz W, Jolly M. Pain scores among emergency department (ED) patients: comparison by ED diagnosis. J Emerg Med 2013;44:46–52.10.1016/j.jemermed.2012.05.002Search in Google Scholar PubMed
[15] Raftery KA, Smith-Coggins R, Chen AH. Gender-associated differences in emergency department pain management. Ann Emerg Med 1995;26:414–21.10.1016/S0196-0644(95)70107-9Search in Google Scholar
[16] McCaffery M, Pasero C. Pain: clinical manual. St. Louis, Missouri: Mosby Incorporated, 1999:93.Search in Google Scholar
[17] Bijur PE, Latimer CT, Gallagher EJ. Validation of a verbally administered Numerical Rating Scale of acute pain for use in the emergency department. Acad Emerg Med 2003;10:390–2.10.1111/j.1553-2712.2003.tb01355.xSearch in Google Scholar PubMed
[18] Pretorius A, Searle J, Marshall B. Barriers and enablers to emergency department nurses’ management of patients’ pain. Pain Manag Nurs 2015;16:372–9.10.1016/j.pmn.2014.08.015Search in Google Scholar PubMed
[19] Manterola C, Vial M, Moraga J, Astudillo P. Analgesia in patients with acute abdominal pain. Cochrane Database Syst Rev 2011:Cd005660.10.1002/14651858.CD005660.pub3Search in Google Scholar PubMed
[20] Ducharme J. Why is improving pain care so hard? Emerg Med Australas 2013;25:110–1.10.1111/1742-6723.12054Search in Google Scholar PubMed
[21] Lewallen S, Courtright P. Epidemiology in practice: case-control studies. Community Eye Health 1998;11:57–8.Search in Google Scholar
©2020 Milan L. Ridderikhof et al., published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.
Articles in the same Issue
- Frontmatter
- Editorial
- Change in Editorship: A Tribute to the Outgoing Editor-in-Chief
- Editorial comments
- Laboratory biomarkers of systemic inflammation – what can they tell us about chronic pain?
- Considering the interpersonal context of pain catastrophizing
- Systematic review
- Altered pain processing and sensitisation is evident in adults with patellofemoral pain: a systematic review including meta-analysis and meta-regression
- Topical reviews
- Pain revised – learning from anomalies
- Role of the immune system in neuropathic pain
- Clinical pain research
- Cryoneurolysis for cervicogenic headache – a double blinded randomized controlled study
- Interpersonal problems as a predictor of pain catastrophizing in patients with chronic pain
- Pain and small-fiber affection in hereditary neuropathy with liability to pressure palsies (HNPP)
- Predicting the outcome of persistent sciatica using conditioned pain modulation: 1-year results from a prospective cohort study
- Observational studies
- Revised chronic widespread pain criteria: development from and integration with fibromyalgia criteria
- The relationship between patient factors and the refusal of analgesics in adult Emergency Department patients with extremity injuries, a case-control study
- Chronic neuropathic pain after traumatic peripheral nerve injuries in the upper extremity: prevalence, demographic and surgical determinants, impact on health and on pain medication
- Tramadol prescribed use in general and chronic noncancer pain: a nationwide register-based cohort study of all patients above 16 years
- Changes in inflammatory plasma proteins from patients with chronic pain associated with treatment in an interdisciplinary multimodal rehabilitation program – an explorative multivariate pilot study
- Original experimental
- The pro-algesic effect of γ-aminobutyric acid (GABA) injection into the masseter muscle of healthy men and women
- The relationship between fear generalization and pain modulation: an investigation in healthy participants
- Experimental shoulder pain models do not validly replicate the clinical experience of shoulder pain
- Computerized quantification of pain drawings
- Head repositioning accuracy is influenced by experimental neck pain in those most accurate but not when adding a cognitive task
- Short communications
- Dispositional empathy is associated with experimental pain reduction during provision of social support by romantic partners
- Superior cervical sympathetic ganglion block under ultrasound guidance promotes recovery of abducens nerve palsy caused by microvascular ischemia
Articles in the same Issue
- Frontmatter
- Editorial
- Change in Editorship: A Tribute to the Outgoing Editor-in-Chief
- Editorial comments
- Laboratory biomarkers of systemic inflammation – what can they tell us about chronic pain?
- Considering the interpersonal context of pain catastrophizing
- Systematic review
- Altered pain processing and sensitisation is evident in adults with patellofemoral pain: a systematic review including meta-analysis and meta-regression
- Topical reviews
- Pain revised – learning from anomalies
- Role of the immune system in neuropathic pain
- Clinical pain research
- Cryoneurolysis for cervicogenic headache – a double blinded randomized controlled study
- Interpersonal problems as a predictor of pain catastrophizing in patients with chronic pain
- Pain and small-fiber affection in hereditary neuropathy with liability to pressure palsies (HNPP)
- Predicting the outcome of persistent sciatica using conditioned pain modulation: 1-year results from a prospective cohort study
- Observational studies
- Revised chronic widespread pain criteria: development from and integration with fibromyalgia criteria
- The relationship between patient factors and the refusal of analgesics in adult Emergency Department patients with extremity injuries, a case-control study
- Chronic neuropathic pain after traumatic peripheral nerve injuries in the upper extremity: prevalence, demographic and surgical determinants, impact on health and on pain medication
- Tramadol prescribed use in general and chronic noncancer pain: a nationwide register-based cohort study of all patients above 16 years
- Changes in inflammatory plasma proteins from patients with chronic pain associated with treatment in an interdisciplinary multimodal rehabilitation program – an explorative multivariate pilot study
- Original experimental
- The pro-algesic effect of γ-aminobutyric acid (GABA) injection into the masseter muscle of healthy men and women
- The relationship between fear generalization and pain modulation: an investigation in healthy participants
- Experimental shoulder pain models do not validly replicate the clinical experience of shoulder pain
- Computerized quantification of pain drawings
- Head repositioning accuracy is influenced by experimental neck pain in those most accurate but not when adding a cognitive task
- Short communications
- Dispositional empathy is associated with experimental pain reduction during provision of social support by romantic partners
- Superior cervical sympathetic ganglion block under ultrasound guidance promotes recovery of abducens nerve palsy caused by microvascular ischemia


