Abstract
Background and aims
While social interactions like verbal support and physical touch have repeatedly been shown to reduce experimental pain, analgesic effects of passive social support, i.e. the sole physical presence of a supportive other, remain unclear. Moreover, little is known about individual factors influencing the extent of pain attenuation during social support. This study investigated analgesic effects of passive support by a romantic partner and the role of partner empathy therein.
Methods
In 48 heterosexual couples, sensitivity to pressure pain was assessed; each participant was tested alone and in the passive presence of his/her partner. Dispositional empathy was quantified by a questionnaire.
Results
In the presence, as compared to absence, of their partners men and women exhibited higher pain threshold and tolerance, as well as lower sensory and affective pain ratings on constant pressure stimuli. Partner empathy was positively associated with pain tolerance and inversely associated with sensory pain experience.
Conclusions
The results confirm the analgesic effects of social support, which may even occur without verbal or physical contact. Partner empathy may buffer affective distress during pain exposure, thereby reducing pain sensitivity and promoting pain coping. These processes may occur solely due to a partner’s physical presence and do not necessarily require direct empathetic feedback.
As a subjective sensory and affective experience, pain varies according to various psychosocial, in addition to physical, variables [1]. Substantial pain modulation through interpersonal factors is illustrated by a decrease of experimental pain responses during support by significant others or strangers. Manipulations like verbal encouragement [2], [3] or hand holding [4], [5] led to reductions in ratings of pain on application of nociceptive stimuli. Even passive social support, i.e. another person’s physical presence without verbal or non-verbal interaction [2], [6], or viewing a photograph of a beloved person, proved successful in pain attenuation [7]. Despite this evidence, it is important to note that analgesic effects of social support vary substantially among individuals, and conflicting findings have also been reported. While in some studies passive support exerted only minimal or no effects [3], [5], in another study women in fact experienced more pain in the presence of a same sex friend than when being tested alone [8].
With the aim of explaining differences in findings, a systematic review identified several factors that may influence interpersonal pain modulation [9], which depends on the degree to which a person in pain can perceive the intentions and opportunities for action of the social partner. In addition, changes in pain may vary according to the characteristics of the relationship between the partners, as well as individual differences in relating to others and coping styles. However, solid evidence of the role of the individual characteristics of the interaction partners is still lacking. Attachment style has been considered relevant in this regard. In women, the effect of unstructured verbal interaction with the spouse depended on attachment anxiety, where pain was strongest when both partners were anxiously attached [10]. Pain catastrophizing has also been assessed, where students scoring high on this variable showed longer pain expressions during passive social support than when being tested alone [11]. Further influencing factors discussed in the literature include perceived everyday social support [8], and preoccupation and solicitousness in romantic couples [12], [13].
To extend our knowledge of the role of individual differences in social pain modulation, the present study aimed to investigate the implications of dispositional empathy, which refers to a stable trait tendency to be aware of, and vicariously experience, the thoughts, feelings and perceptions of another [14]. While empathy is a relevant predictor of social support provision [15], its role in the social context of pain is still poorly understood [9]. While two studies documented changes in pain perception due to experimental manipulation of empathetic feedback [16], [17], only one addressed individual differences in dispositional empathy [5]; it revealed greater pain reduction during partner hand-holding in women with more empathetic partners.
Building on this finding, we investigated the effects of empathy on pain modulation via passive social support of romantic partners of both genders. Potential mechanisms mediating such effects include vicarious effects of pain observation, in addition to emotional modulation of pain experience. In the sense of emotional contagion, observing pain in another individual triggers negative feelings, and even similar states in the central and autonomic nervous systems of the observer [18]. Receiving empathetic feedback may diminish distress in a suffering individual, which in turn may lead to pain reduction [19]. It is likely that this effect is greater if a partner tends towards stronger empathetic responses. During passive support, empathy may not be communicated verbally or by physical touch; however, ongoing experience of high partner empathy in everyday life may generalize to a pain situation, in which the presence of the partner may attenuate pain even if she/he behaves passively. Based on these consideration, we hypothesized that (1) the pain response to nociceptive stimulation would be smaller during presence than absence of a passively behaving partner, and that (2) pain reduction would be stronger if the partner exhibits higher dispositional empathy.
Forty-eight heterosexual couples participated (mean age: 25.40 years, SD=5.18 years; mean partnership duration 3.22 years, SD=3.84 years). The sample size was determined based on previous studies regarding the effects of passive social support on pain, most of which revealed effects sizes in the medium range. None of the participants was suffering from acute or chronic pain of any kind or was taking analgesic medication. Participants were tested in equal proportions at UMIT – University of Health Sciences Medical Informatics and Technology (Austria) and the University of the Balearic Islands (Spain). They were recruited via email lists of the universities.
A pressure algometer (FPN 300, Wagner Instruments, Greenwich, CT, USA) was used for pain quantification. The device has a 1 cm2 rubber tip and was fixed in a movable mounting, which allowed precise manual pressure adjustment. Pressure pain threshold and tolerance were quantified using a testing-the-limits procedure. For this purpose, pressures were applied to the nail of the index finger of the non-dominant hand with a rate of increase of 0.1 kg/s. Subjects were instructed to give a stop signal as soon as they noticed the first pain sensation (pain threshold) or could no longer tolerate the pain (pain tolerance) (three trials each for threshold and tolerance). Moreover, pain ratings on constant pressure stimuli (3 kg, 30 s) were obtained. Pain sensations were quantified using two 10 cm visual analogue scales (VAS). They provided measures of sensory pain (“How strong was the pain?”), and affective pain (“How unpleasant was the pain?”).
Using a cross-over design, pain assessments were conducted twice in each participant, i.e. in the presence and absence of his/her partner. During the presence condition, partners were sitting together at a table at a distance of approximately 1 m from each other; they were able to make eye contact, but were instructed not to talk to each other during the entire procedure. During the absence condition, one of the partners had to leave the room. The sequence of testing (first in presence vs. first in absence of the partner) was randomized across genders. After pain testing, participants were presented with the Saarbrucken Personality Questionnaire on Empathy (SPQE) [20], which quantifies cognitive and emotional aspects of dispositional empathy based on 16 items. The Cronbach’s α of the SPQE sum score is 0.76; its validity is supported by substantial correlations with other questionnaires assessing empathy [20]. The partners completed the questionnaires separately from one another, i.e. without verbal or visual contact. All assessments were conducted by a female experimenter. The study was approved by the institutional ethics board of the Institute of Psychology of UMIT – University of Health Sciences Medical Informatics and Technology (approval number: LN120717). All participants provided their informed consent. In addition to information about the methods applied, the informed consent form included the statement that the purpose of the study was to investigate the effects of the presence of one’s partner on pain perception.
To analyze the effects of experimental conditions (partner presence vs. absence) on pain perception (hypothesis 1), one-way ANOVAs were conducted with the threshold measures (means of the three trials) and VAS ratings as dependent variables. To test whether the difference between the conditions varies according to partner empathy (hypothesis 2), and to explore possible gender effects on pain, mixed ANCOVAs were computed with condition as a within-subject factor, gender as a between-subjects factor and the SPQE sum score of the corresponding partner as a covariate.
During presence (as compared to absence) of their partners, men and women exhibited higher pain threshold and tolerance, as well as lower VAS ratings on sensory and affective pain (Figs. 1 and 2). Medium to large effects were seen in the one-way ANOVAs (threshold, F[1], 95]=11.79, p=0.001,
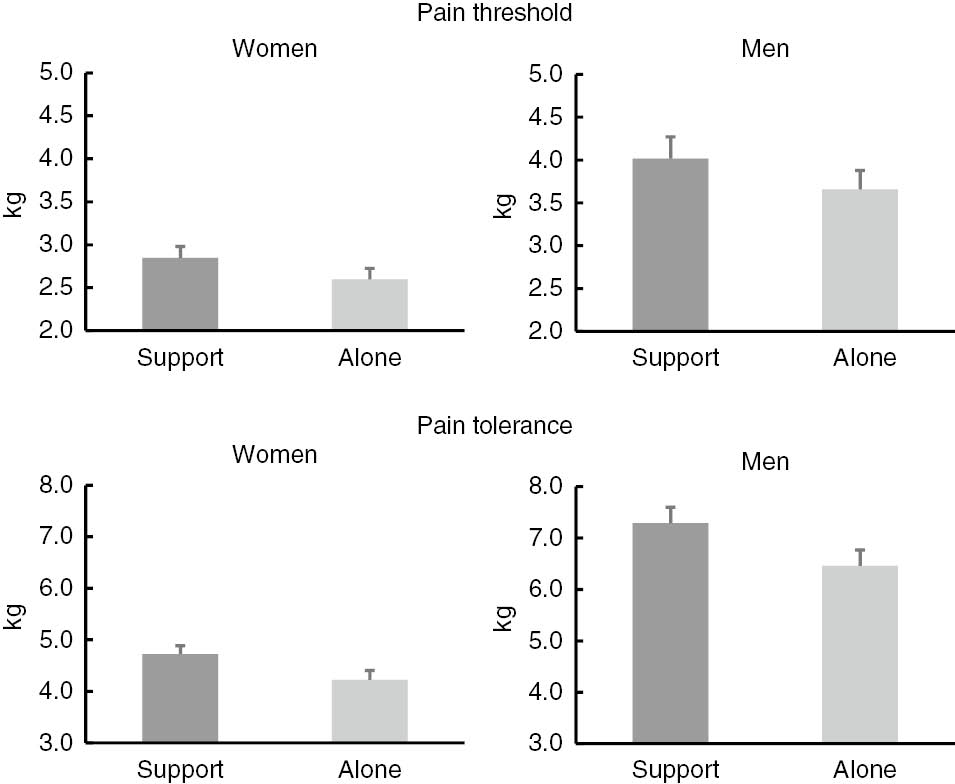
Pain threshold and pain tolerance during both experimental conditions.
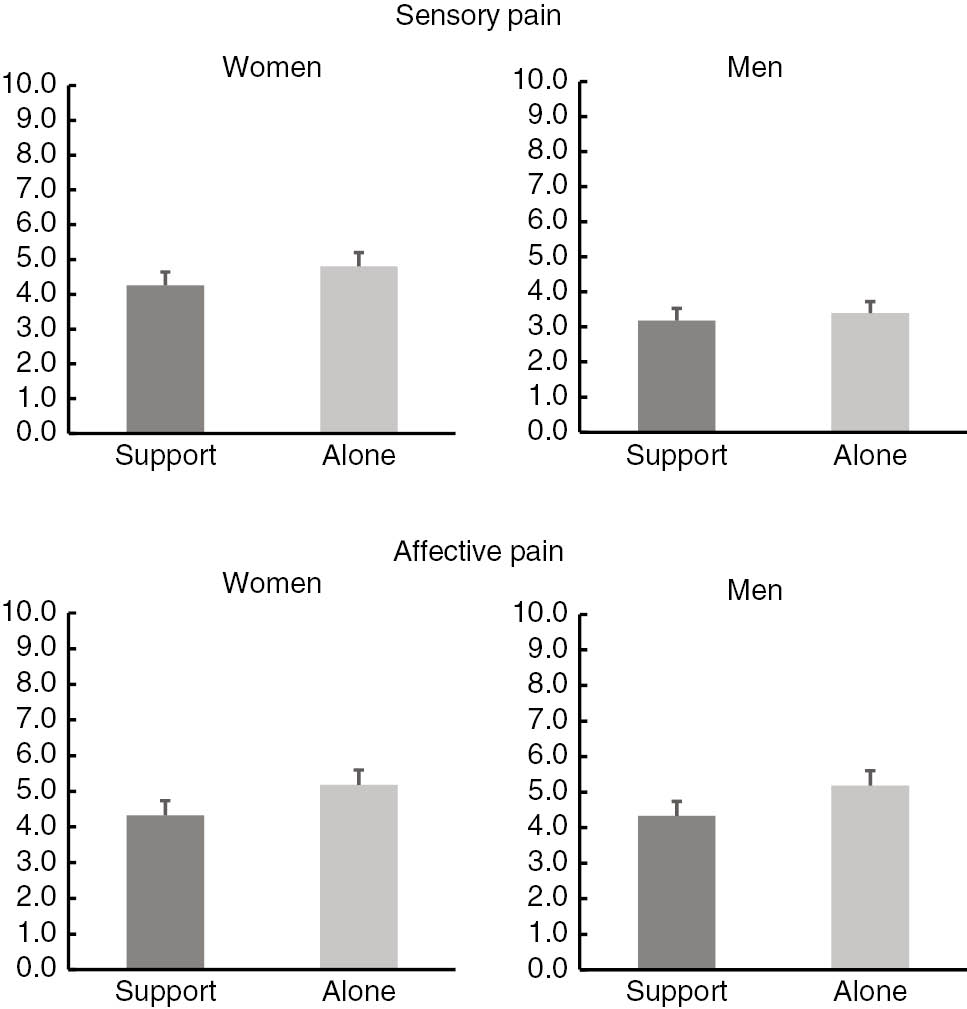
VAS ratings on constant pressure stimulation during both experimental conditions.
The result supports the notion of substantial attenuation of experimental pain due to social support, which may even occur during conditions of minimal interaction, i.e. without verbal or physical contact. This accords with earlier reports of reduced cold pressor pain during passive social support [2], [6]. However, other studies did not reveal significant differences in pain sensitivity between subjects tested alone and during the presence of a passively behaving romantic partner [5] or unfamiliar person [3]. This divergence may be at least partly explained by different methodologies: in contrast to automatized procedures, used for example for painful heat stimulation [5], the procedure of pain testing in our study involved some degree of social contact between the participant and the experimenter. It may be that the interactive component of this procedure had a (social) influence on pain perception.
The interactions observed in the ANCOVAs indicate that participants whose partners reported greater dispositional empathy exhibited a larger increase of pain tolerance, and larger reduction of sensory pain, during partner presence. While a positive correlation between partner empathy and experimental pain was previously reported during hand holding [5], the present study is the first to demonstrate such an association during passive social support. This observation is in line with the effects of experimentally applied empathetic feedback: empathetic comments during nociceptive stimulation were associated with lower reported pain than were unempathetic and neutral comments [16]. Moreover, explicit instruction to take the perspective of a romantic partner subjected to painful stimulation also led to pain attenuation [17]. It has been claimed that empathetic feedback to a partner experiencing pain may promote intimacy and closeness and reduce perceived threat, thereby facilitating emotion regulation and diminishing distress [17], [19]. More positive emotional states are in turn associated with reduced pain sensitivity and improved pain coping [21]. Importantly, in our study partner empathy was related to pain perception, even though the interaction was limited to visual contact and participants did not receive direct supportive feedback. It may be argued that day-to-day experience with a highly empathetic partner leads to a general expectation of his or her compassion and emotional support in threatening situations; as such, the sole presence of the partner may reduce distress and pain sensitivity.
However, it should not be overlooked that the association with empathy was restricted to modulation of pain tolerance and sensory pain experience; in particular, the lack of an association with affective pain is difficult to explain. It also has to be noted that no measure of perceived social support was obtained in the study. As such, the possibility that pain reduction to some extent was due to distraction caused by the mere presence of the partner, instead of actual support, cannot be ruled out. Another limitation pertains to the exclusive use of a female experimenter, where differential experimenter effects on both genders cannot be ruled out. Specifically, men tend to report lower pain intensities to female as opposed to male experimenters [22]. In addition, some relevant variables characterizing the partnerships may not have been assessed, such as partnership satisfaction, intimacy, trust or attachment style.
Despite these restrictions, the study provided evidence that the presence of a romantic partner is effective in reducing acute pain even without his or her active feedback, and that this effect increases with partner empathy. The results contrast with the model of operant learning, according to which sympathetic partner behaviors may enhance pain and pain-related behaviors due to positive reinforcement [23]. There is indeed substantial evidence in the context of chronic pain that solicitous partner behaviours are associated with greater patient disability [23]. However, it is important to note that solicitousness is not identical to empathic responses involving validation, i.e. understanding, adequacy and acceptance of the partner’s behaviour [24]. Validating responses of a partner in turn were shown to be associated with a reduction of negative affect in pain patients [24]. In conclusion, our findings underline the beneficial role of social support in pain relief and encourage use of interpersonal strategies in behavioral approaches to pain management.
Access to research data
The research data of the study are available to the public via the repository Open Science Framework (OSF: https://osf.io/58b7y/).
-
Authors’ statements
-
Research funding: Authors state no funding involved.
-
Conflict of interest: Authors state no conflict of interest.
-
Informed consent: Informed consent has been obtained from all individuals included in this study.
-
Ethical approval: The research related to human use complies with all the relevant national regulations, institutional policies and was performed in accordance with the tenets of the Helsinki Declaration, and has been approved by the authors’ institutional review board.
References
[1] McMahon S, Koltzenburg M, Tracey I, Turk D. Wall & Melzack’s textbook of pain, 6th ed. Oxford: Elsevier, 2013.Search in Google Scholar
[2] Brown JL, Sheffield D, Leary MR, Robinson ME. Social support and experimental pain. Psychosom Med 2003;65:276–83.10.1097/01.PSY.0000030388.62434.46Search in Google Scholar
[3] Roberts MH, Klatzkin RR, Mechlin B. Social support attenuates physiological stress responses and experimental pain sensitivity to cold pressor pain. Ann Behav Med 2015;49:557–69.10.1007/s12160-015-9686-3Search in Google Scholar PubMed
[4] Coan JA, Schaefer HS, Davidson RJ. Lending a hand: social regulation of the neural response to threat. Psychol Sci 2006;17:1032–9.10.1111/j.1467-9280.2006.01832.xSearch in Google Scholar PubMed
[5] Goldstein P, Shamsay-Tsoory SG, Yellinek S, Weissman-Fogel I. Empathy predicts an experimental pain reduction during touch. J Pain 2016;17:1049–57.10.1016/j.jpain.2016.06.007Search in Google Scholar PubMed
[6] Edwards R, Eccleston C, Keogh E. Observer influences on pain: an experimental series examining same-sex and opposite-sex friends, strangers, and romantic partners. Pain 2017;158:846–55.10.1097/j.pain.0000000000000840Search in Google Scholar PubMed
[7] Eisenberger NI, Master SL, Inagaki TK, Taylor SE, Shirinyan D, Lieberman MD, Naliboff BD. Attachment figures activate a safety signal-related neural region and reduce pain experience. Proc Natl Acad Sci U S A 2011;108:11721–6.10.1073/pnas.1108239108Search in Google Scholar PubMed PubMed Central
[8] McClelland LE, McCubbin JA. Social influence and pain response in women and men. J Behav Med 2008;31:413–20.10.1007/s10865-008-9163-6Search in Google Scholar PubMed
[9] Krahé C, Springer A, Weinman JA, Fotopoulou A. The social modulation of pain: Others as predictive signals of salience – a systematic review. Front Hum Neurosci 2013;7:368.10.3389/fnhum.2013.00386Search in Google Scholar PubMed PubMed Central
[10] Wilson CL, Ruben MAA. A pain in her arm: romantic attachment orientations and the tourniquet task. Pers Relatsh 2011;18:242–65.10.1111/j.1475-6811.2011.01359.xSearch in Google Scholar
[11] Sullivan MJL, Adams H, Sullivan ME. Communicative dimensions of pain catastrophizing: social cueing effects on pain behaviour and coping. Pain 2004;107:220–6.10.1016/j.pain.2003.11.003Search in Google Scholar PubMed
[12] Flor H, Breitensteiner C, Birbaumer N, Fürst M. A psychophysiological analysis of spouse solicitousness towards pain behaviours, spouse interaction, and pain perception. Behav Ther 1995;26:255–77.10.1016/S0005-7894(05)80105-4Search in Google Scholar
[13] Nilakantan A, Younger J, Aron A, Mackey S. Preoccupation in an early-romantic relationship predicts experimental pain relief. Pain Med 2014;15:947–53.10.1111/pme.12422Search in Google Scholar PubMed PubMed Central
[14] Eisenberg N, Eggum ND, Di Giunta L. Empathy-related responding: Associations with prosocial behavior, aggression, and intergroup relations. Soc Issues Policy Rev 2010;4: 143–80.10.1111/j.1751-2409.2010.01020.xSearch in Google Scholar PubMed PubMed Central
[15] Devoldre I, Davis MH, Verhofstadt LL, Buysse A. Empathy and social support provision in couples: social support and the need to study the underlying processes. J Psychol 2010;144:259–84.10.1080/00223981003648294Search in Google Scholar PubMed
[16] Fauchon C, Faillenot I, Perrin AM, Borg C, Pichot V, Chouchou F, Garcia-Larrea L, Peyron R. Does an observer’s empathy influence my pain? Effect of perceived empathetic or unempathetic support on a pain test. Eur J Neurosci 2017;46:2629–37.10.1111/ejn.13701Search in Google Scholar PubMed
[17] Leong LE, Cano A, Wurm LH, Lumley MA, Corley AM. A perspective-taking manipulation leads to greater empathy and less pain during the cold pressor task. J Pain 2015;16: 1176–85.10.1016/j.jpain.2015.08.006Search in Google Scholar PubMed
[18] Mailhot JP, Vachon-Presseau E, Jackson PL, Rainville P. Dispositional empathy modulates vicarious effects of dynamic pain expressions on spinal nociception, facial responses and acute pain. Eur J Neurosci 2012;35:271–8.10.1111/j.1460-9568.2011.07953.xSearch in Google Scholar PubMed
[19] Edmond SN, Keefe FJ. Validating pain communication: current state of the science. Pain 2015;156:215–9.10.1097/01.j.pain.0000460301.18207.c2Search in Google Scholar PubMed PubMed Central
[20] Paulus C. The Saarbrueck personality questionnaire on empathy: psychometric evaluation of the German version of the International Reactivity Index. 2009; Available at: http://hdl.handle.net/20.500.11780/3343. Accessed: 5 Feb 2019.Search in Google Scholar
[21] Meagher MW, Arnau RC, Rhudy JL. Pain and emotion: effects of affective picture modulation. Psychosom Med 2001;63:79–90.10.1097/00006842-200101000-00010Search in Google Scholar PubMed
[22] Aslaksen PM, Myrbakk IN, Hoifodt RS, Flaten MA. The effect of experimenter gender on autonomic and subjective responses to pain stimuli. Pain 2007;129:260–8.10.1016/j.pain.2006.10.011Search in Google Scholar PubMed
[23] Newton-John TRO. Solicitousness and chronic pain: a critical review. Pain Reviews 2002;9:7–27.10.1191/0968130202pr186raSearch in Google Scholar
[24] Edlund SM, Carlsson ML, Linton SJ, Fruzzetti AE, Tillfors M. I see you’re in pain – the effects of partner validation on emotions in people with chronic pain. Scand J Pain 2015;6:16–21.10.1016/j.sjpain.2014.07.003Search in Google Scholar PubMed
©2020 Scandinavian Association for the Study of Pain. Published by Walter de Gruyter GmbH, Berlin/Boston. All rights reserved.
Articles in the same Issue
- Frontmatter
- Editorial
- Change in Editorship: A Tribute to the Outgoing Editor-in-Chief
- Editorial comments
- Laboratory biomarkers of systemic inflammation – what can they tell us about chronic pain?
- Considering the interpersonal context of pain catastrophizing
- Systematic review
- Altered pain processing and sensitisation is evident in adults with patellofemoral pain: a systematic review including meta-analysis and meta-regression
- Topical reviews
- Pain revised – learning from anomalies
- Role of the immune system in neuropathic pain
- Clinical pain research
- Cryoneurolysis for cervicogenic headache – a double blinded randomized controlled study
- Interpersonal problems as a predictor of pain catastrophizing in patients with chronic pain
- Pain and small-fiber affection in hereditary neuropathy with liability to pressure palsies (HNPP)
- Predicting the outcome of persistent sciatica using conditioned pain modulation: 1-year results from a prospective cohort study
- Observational studies
- Revised chronic widespread pain criteria: development from and integration with fibromyalgia criteria
- The relationship between patient factors and the refusal of analgesics in adult Emergency Department patients with extremity injuries, a case-control study
- Chronic neuropathic pain after traumatic peripheral nerve injuries in the upper extremity: prevalence, demographic and surgical determinants, impact on health and on pain medication
- Tramadol prescribed use in general and chronic noncancer pain: a nationwide register-based cohort study of all patients above 16 years
- Changes in inflammatory plasma proteins from patients with chronic pain associated with treatment in an interdisciplinary multimodal rehabilitation program – an explorative multivariate pilot study
- Original experimental
- The pro-algesic effect of γ-aminobutyric acid (GABA) injection into the masseter muscle of healthy men and women
- The relationship between fear generalization and pain modulation: an investigation in healthy participants
- Experimental shoulder pain models do not validly replicate the clinical experience of shoulder pain
- Computerized quantification of pain drawings
- Head repositioning accuracy is influenced by experimental neck pain in those most accurate but not when adding a cognitive task
- Short communications
- Dispositional empathy is associated with experimental pain reduction during provision of social support by romantic partners
- Superior cervical sympathetic ganglion block under ultrasound guidance promotes recovery of abducens nerve palsy caused by microvascular ischemia
Articles in the same Issue
- Frontmatter
- Editorial
- Change in Editorship: A Tribute to the Outgoing Editor-in-Chief
- Editorial comments
- Laboratory biomarkers of systemic inflammation – what can they tell us about chronic pain?
- Considering the interpersonal context of pain catastrophizing
- Systematic review
- Altered pain processing and sensitisation is evident in adults with patellofemoral pain: a systematic review including meta-analysis and meta-regression
- Topical reviews
- Pain revised – learning from anomalies
- Role of the immune system in neuropathic pain
- Clinical pain research
- Cryoneurolysis for cervicogenic headache – a double blinded randomized controlled study
- Interpersonal problems as a predictor of pain catastrophizing in patients with chronic pain
- Pain and small-fiber affection in hereditary neuropathy with liability to pressure palsies (HNPP)
- Predicting the outcome of persistent sciatica using conditioned pain modulation: 1-year results from a prospective cohort study
- Observational studies
- Revised chronic widespread pain criteria: development from and integration with fibromyalgia criteria
- The relationship between patient factors and the refusal of analgesics in adult Emergency Department patients with extremity injuries, a case-control study
- Chronic neuropathic pain after traumatic peripheral nerve injuries in the upper extremity: prevalence, demographic and surgical determinants, impact on health and on pain medication
- Tramadol prescribed use in general and chronic noncancer pain: a nationwide register-based cohort study of all patients above 16 years
- Changes in inflammatory plasma proteins from patients with chronic pain associated with treatment in an interdisciplinary multimodal rehabilitation program – an explorative multivariate pilot study
- Original experimental
- The pro-algesic effect of γ-aminobutyric acid (GABA) injection into the masseter muscle of healthy men and women
- The relationship between fear generalization and pain modulation: an investigation in healthy participants
- Experimental shoulder pain models do not validly replicate the clinical experience of shoulder pain
- Computerized quantification of pain drawings
- Head repositioning accuracy is influenced by experimental neck pain in those most accurate but not when adding a cognitive task
- Short communications
- Dispositional empathy is associated with experimental pain reduction during provision of social support by romantic partners
- Superior cervical sympathetic ganglion block under ultrasound guidance promotes recovery of abducens nerve palsy caused by microvascular ischemia


