Abstract
Background
The aim of the present study was to compare hemoglobin (Hb) levels determined by point-of-care testing (POCT) HemoCue® and arterial blood gas analyzer using an automated hematology analyzer in critically ill geriatric patients.
Methods
Forty geriatric patients requiring intensive care treatment were included in the study. Arterial blood sample was analyzed using HemoCue® (HemoCue®; Hb 201+, Angelholm, Sweden) (HbHemoCueArterial), blood gas analyzer (Techno Medica, Gastat1800 series, Japan) (HbBGA) and an automated hematology analyzer (Cell Dyne 3700 System, Abbott Laboratories, USA) (HbLab) as a reference method. Capillary blood measurements were performed (HbHemoCueCapillary) using HemoCue® at bedside. Bland-Altman analysis was applied to the results.
Results
We found a positive correlation between the Hb measurements of HemoCueCapillary, HemoCueArterial and automated hematology analyzer (r-values were 0.799 and 0.922, respectively) and p<0.001. There was also a positive correlation between the Hb measurements of blood gas analyzer and automated hematology analyzer (r = 0.878) and p<0.001. The bias and limits of agreement were 0.32 and −2.5±3.14 g/dL for the HbHemoCueCapillary, 0.64 and −1.03±2.31 g/dL for the HbHemoCueArterial and −1.2 and −4.45±2.05 g/dL for the HbBGA. Inotropic agent administration did not affect the Hb values in all groups.
Conclusions
Both HemoCueCapillary and HemoCueArterial are sufficiently accurate and correlated with automated hematology analyzer in geriatric critically ill patients if used correctly. In terms of Hb levels, arterial and capillary blood sample measurements with HemoCue® provided more clinically acceptable accuracy than blood gas analysis system.
Introduction
The etiology of anemia is multifactorial in the intensive care unit (ICU). The causes of anemia are the changes in iron metabolism, hemodilution, hemorrhage, increased red cell destruction, bone marrow suppression and reduced action of erythropoietin [1, [2]. Vincent et al. reported that if the patients stay longer than 7 days in the ICU, they had a red blood cell transfusion rate of 73% 3]. Also, diagnostic blood loss due to phlebotomy and repetitive laboratory testing is another important factor causing blood loss [4]. The impact of anemia in the elderly patients increases the mortality and morbidity in the ICU due to hemodynamic disorders, cardio-respiratory complications, confusion and cognitive decline and falls [5]. The International Committee for Standardization in Hematology recommends an automated analyzer as the gold standard for hemoglobin (Hb) measurement in the clinical laboratory [6]. However, the test reporting time may be delayed in the period between the drawing of blood and laboratory analysis. Point-of-care testing (POCT) devices can be operated using small sample volumes with a brief training. HemoCue® is a portable analyzer that uses the azide-met-Hb reaction and photometry. Only a drop of blood (10 μL) is placed on a cuvette and the device displays the Hb concentration in 15–60 s [7]. Arterial blood gas analyzers provide rapid analysis of traditional blood gas elements such as PH, PO2 and also Hb concentration. Cell Dyne 3700 is an automated hematology analyzer which is defined as the gold standard in clinical laboratories. The aim of this study was to determine the accuracy of HemoCueCapillary, HemoCueArterial and blood gas analyzer for Hb measurement and compare it with that of the automated laboratory analyzer in geriatric patients requiring intensive care. We also investigated whether capillary or arterial blood sample made a difference in the measurement with HemoCue®.
Materials and methods
The trial was registered at http://www.clinicaltrials.gov (NCT03509987). Approval for this study was obtained from the Local Ethical Committee and the study was conducted in the ICU of Kecioren Training and Research Hospital, Ankara, Turkey. We accepted patients as geriatric if they were ≥65 years old. Forty patients with ages 65 years and older who required Hb analysis in the intensive care treatment were enrolled in this prospective study. Invasive arterial pressure was monitored in all the patients. The Hb level of each subject was recorded using four different methods: HbHemoCueArterial, HbHemoCueCapillary, HbBGA and HbLab. Arterial blood sample was obtained from each patient via an arterial line. After eliminating the tubing dead space, arterial blood was drawn in a 10 mL syringe and a portion of this sample was placed into a 2.5 mL heparinized syringe and analyzed using a blood gas analyzer (Techno Medica, Gastat 1800 series, Yokohama, Kanagawa, Japan) (HbBGA). The absorption of the Hb derivatives measured at specific wavelengths is directly proportional to their concentration. In the blood gas analyzer, 120 μL blood is needed for analysis and the device displays the Hb concentration in approximately 50 s.
Arterial blood sample of 2.5 mL was placed in an appropriate tube containing ethylenediamine tetraacetic acid (EDTA) for a complete blood count (CBC) in the automated hematology analyzer. The automated hematology analyzer (Cell Dyne 3700 System, Abbott Laboratories, IL, USA) was defined as the gold standard for Hb measurement in this study (HbLab). The remaining arterial blood sample was analyzed with HemoCue (HemoCue® Hb 201+, Angelholm, Sweden [HbHemoCueArterial]). At the same time, capillary blood sample for Hb measurement with the HemoCue (HemoCue® Hb 201+, Angelholm, Sweden) (HbHemoCueCapillary) was obtained from the finger punctures of non-intravenous fluid infusion site after cleaning the sampling point. The first three drops of blood were wiped away. The fourth drop was used for the cuvette photometry. The presence of air bubbles was assessed before administering the blood sample into the device and 10 μL blood was used for the capillary analysis with HemoCue®. Patient characteristics, norepinephrine administration, peripheral edema at the sampling site, the reason for the patients’ admission to the ICU were recorded. The presence of edema was based on “pitting”. We used a grading system. The severity of bilateral pitting edema was defined as: 1+ (mild): both feet/ankles; 2+ (moderate): both feet, lower legs, hands or lower arms; 3+ (severe): generalized bilateral pitting edema, including both feet, legs, arms and face.
Statistical analysis was performed using SPSS 22.0 (SPSS Inc., Chicago, IL, USA). Agreements between HbHemoCueArterial, HbHemoCueCapillary, HbBGA and HbLab were assessed by the method of Bland-Altman, calculating the bias (mean difference) and limits of agreement (bias±1.96*standard deviation [SD]). The automated whole blood analyzer was considered as the gold standard and the Pearson’s correlation coefficient (r) was calculated to assess the correlation with HbHemoCueArterial, HbHemoCueCapillary and HbBGA. p<0.05 was considered statistically significant.
Results
Forty critically ill patients, 15 men (37.5%) and 25 women (62.5%) of ages 65 years and older were enrolled in the study. The mean±SD value of age was 74.7±8.9, 65% of the patients were in the postoperative period, 15% had neurologic disorders (cerebrovascular infarct, hemorrhage), 5% had cardiovascular disorder and 15% had sepsis. Eight patients (20%) were receiving norepinephrine. Fifteen patients (37.5%) needed mechanical ventilation. Only four patients (10%) had moderate pitting edema at the sampling site. The characteristics of the patients are presented in Table 1.
Characteristics of patients.
| Patients | n=40 |
|---|---|
| Age, years | 74.7±8.9 |
| Sex ratio (M/F) | 15/25 |
| Postoperative (orthopedic, abdominal, trauma surgery) | 26 (65%) |
| Neurologic disorder | 6 (15%) |
| Cardiovascular disorder | 2 (5%) |
| Sepsis | 6 (15%) |
| Inotrope administration | 8 (20%) |
| Peripheral edema | 4 (10%) |
| Mechanical ventilation | 15 (37.5%) |
The sample size was set to a minimum of 150 measurements (40 patients each 3–4 measurements) according to Bland and Altman recommendations for a precision of 0.3 SD of the 95% confidence interval (CI) of the limits of agreement [8].
The mean HbHemoCueArterial, HbHemoCueCapillary, HbBGA and HbLab were 10.12±1.9 g/dL, 10.44±2.3 g/dL, 11.9±3.2 g/dL and 10.7±2.1 g/dL, respectively. The bias between HbHemoCueArterial and HbLab was 0.64 g/dL and the limits of agreement were −1.03±2.31 g/dL (Figure 1). There was a significant correlation between HbHemoCueArterial and the reference HbLab (r=0.922, p<0.001).
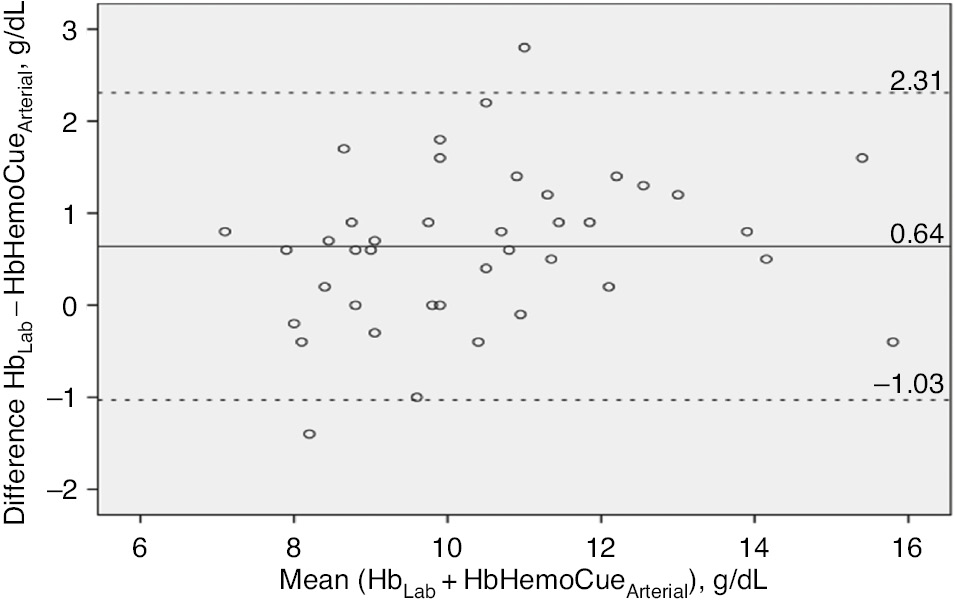
Bland-Altman representation of the bias and the limits of agreement between HbLab and HbHemoCueArterial.
The middle horizontal line represents the bias (mean difference) and the outer lines represent the limits of agreement.
The bias between HbHemoCueCapillary and HbLab was 0.32 g/dL and the limits of agreement were −2.5±3.14 g/dL (Figure 2). There was a significant correlation between HbHemoCueCapillary and the reference HbLab (r=0.799, p<0.001).
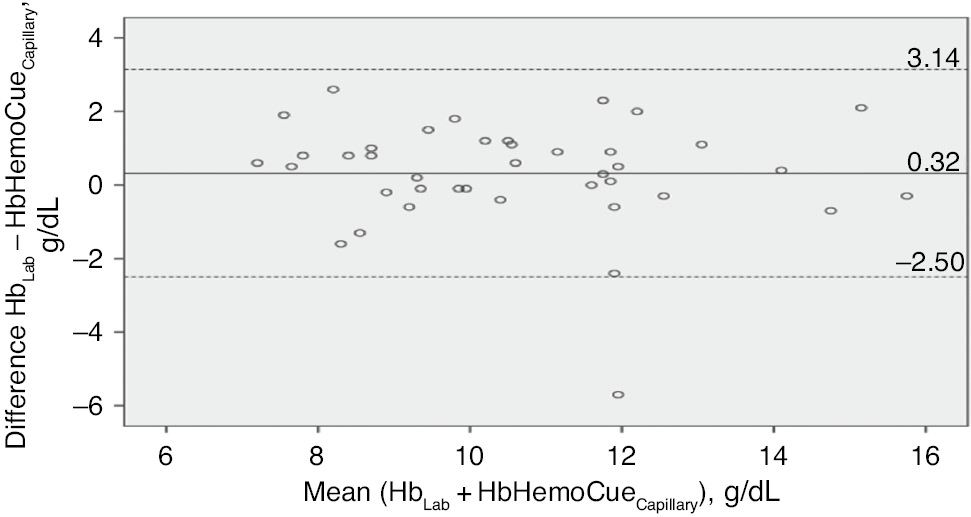
Bland-Altman representation of the bias and the limits of agreement between HbLab and HbHemoCueCapillary.
The middle horizontal line represents the bias (mean difference) and the outer lines represent the limits of agreement.
The bias between HbBGA and HbLab was −1.20 g/dL and the limits of agreement were −4.45±2.05 g/dL (Figure 3). There was a significant correlation between HbBGA and the reference HbLab (r=0.878, p<0.001). Bland-Altman analysis showed a better agreement of HbHemoCueArterial and HbHemoCueCapillary with HbLab than the agreement of HbBGA with HbLab.
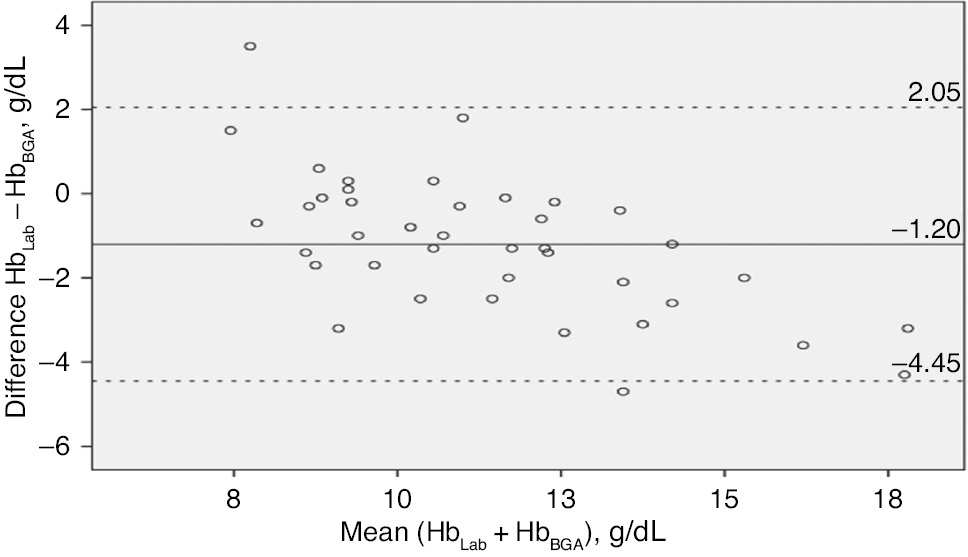
Bland-Altman representation of the bias and the limits of agreement between HbLab and HbBGA.
The middle horizontal line represents the bias (mean difference) and the outer lines represent the limits of agreement.
There was a positive correlation between HemoCueArterial and HemoCueCapillary (r=0.83, p=0.001).
Both the POCT systems were not affected by the norepinephrine administration (p>0.05). Peripheral edema at the sampling site had an effect on HemoCueArterial, HbHemoCueCapillary and HbBGA (p<0.05). Only HbLab was not affected from peripheral edema at the sampling site (p=0.1).
Discussion
Anemia has been significantly associated with mortality in older adults [9]. Anemia is a common complication because of blood losses due to acute traumatic hemorrhages in the postoperative period, due to chronic diseases, liver dysfunction, repeated blood extractions, disseminated intravascular coagulation (DIC), iron or other deficiency disorders among others in the ICU [3]. In this prospective study, we found that HemoCue® cuvette photometry test procedures showed a good correlation with the gold standard laboratory test. These results show that the HemoCue® can be recommended for use in geriatric patients without peripheral edema for Hb estimation in the ICU. To to the best of our knowledge, there have been no published studies investigating the accuracy of POCT in geriatric intensive care patients.
Riessen et al. found that critically ill ICU patients are at high risk for iatrogenic blood loss and development of anemia [10]. In a recent study, Lelubre and Vincent demonstrated that blood transfusions could have a negative impact on the treatment course of ICU patients causing increased mortality [11]. Anemia is a multifactorial process in the ICU and iatrogenic blood loss contributes to about 20% of the total blood loss 2]. For this reason, it is important to diagnose blood loss in a short time by determining Hb levels in geriatric patients.
Hb measurement with an automated whole blood laboratory analyzer is the gold standard for the measurement of Hb concentration providing supplemental diagnostic information such as platelet and white blood cell (WBC) counts. The disadvantage of this technique is the delay in obtaining the results. The time required for blood sampling (venous or arterial), transport to the laboratory, analysis of the blood sample, validation of the measurement and return of the results to the physician with the laboratory analysis is longer than that required for the POCT devices [12]. All of this procedure takes about 60 min in our hospital. HemoCue® and blood gas analysis system report the Hb levels in shorter than 1 min. Also obtaining blood sample from the capillary site is an easy and non-traumatic way than venous or arterial line. Another advantage of HemoCue® is that the determination of Hb level by HemoCue® is a cost-effective and easily used procedure than the automated laboratory measurements [13].
Seguin et al. compared the Hb values of the patients in the ICU determined by the HemoCue® and automated laboratory analyzer. The authors did not recommend the use of HemoCue® for Hb measurement when capillary blood samples are used in the presence of edema [14]. In the present study, four patients (10%) had moderate pitting edema at the sampling site and these edematous patients were hypoalbuminemic. Patients with an albumin level of 3.4 g/dL or less were considered hypoalbuminemic.
Hb values of HemoCueArterial, HemoCueCapillary and BGA were affected from the peripheral edema compared with the automated laboratory analyzer. Laboratory Hb estimations using the Cell Dyne System are based on alterations in electrical impedance. It is possible that by increasing sample conductivity, hypoalbuminemia in these edematous patients caused bias in the “gold standard” automated laboratory measurements rather than in the HemoCue® or BGA measurements. The number of the patients in the study by Seguin et al. was more than that in our study. Only four patients had moderate pitting edema in the present study. For this reason, it cannot be considered as statistically meaningful. We estimated that peripheral edema at the sampling site can have an effect on Hb measurement while using POCT devices. Further studies are required for clearer information about the effect of peripheral edema on POCT systems.
In another study, Mimoz et al. found that arterial HemoCue® was more reliable than capillary HemoCue® to make a therapeutic decision such as whether a blood transfusion should be performed. However, the authors did not investigate the effect of edema on the HemoCue® accuracy [15]. In contrast to these studies, Van de Louw et al. compared capillary HemoCue® with laboratory determination of Hb in patients with gastrointestinal bleeding and they demonstrated that capillary determination of Hb with HemoCue® was useful in the management of patients with gastrointestinal bleeding in the ICU [16]. Similarly, in another study, no significant difference was found between capillary and venous HemoCue® values of 247 primary care patients [17]. In our study, we observed a bias of 0.32 g/dL (95% CI −2.5 to 3.14g/dL) between HbHemoCueCapillary and HbLab. We observed a bias of 0.66 (95% CI −1.03 to 2.31) between HbHemoCueArterial and HbLab. Our results are in accordance with these studies. We aimed to assess the reliability of Hb values in geriatric patients requiring intensive care with POCT systems compared with the reference method. The variability for capillary blood samples may have been affected by the quality of capillary blood drawing. For this reason in the present study, capillary samples were obtained after the finger puncture and the fourth blood drop was used to fill the microcuvette of HemoCue. Although Bland-Altman analysis showed a better agreement of HemoCueArterial and HbHemoCueCapillary with HbLab than the agreement of HbBGA with HbLab, the results of our study cannot be extended to all available blood gas analysis systems.
The blood gas analyzer system needs to be regularly serviced and efficiently controlled for reliable test results. Also, dry heparinized syringes should be preferred for measurements [13]. Capillary and arterial blood sample collection and measurements were done by the same trained physician in our study to prevent technical problems. We used dry heparinized syringes but further studies are needed comparing POCT devices with the automated laboratory analyzer.
Although a positive correlation was found between the Hb measurements of HemoCueCapillary, blood gas analyzer and automated hematology analyzer, the wide limits of agreement mean clinicians should be careful when making clinical decisions based on the results of these devices. Errors in blood sampling handling such as excess blood outside of microcuvette or samples containing air bubbles or not immediately placed in the HemoCue® device may cause inaccurate results [18]. Also peripheral edema at the sampling site and large volume fluid administration may explain the variability of the findings between the studies. The wide limits of agreement observed in HemoCueCapillary may be the result of the errors in blood sampling handling.
In this study, we found that Hb measurement in geriatric ICU patients by HemoCue® was more accurate than by the blood gas analysis system in comparison with automated laboratory measurements. We recommend that HemoCue® can be used in geriatric ICU patients without peripheral edema to measure the Hb levels with a short analysis time and small amount of blood sample when used correctly.
Author contributions: All the authors have accepted responsibility for the entire content of this submitted manuscript and approved submission.
Research funding: None declared.
Employment or leadership: None declared.
Honorarium: None declared.
Competing interests: The funding organization(s) played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the report for publication.
References
1. Shander A. Anemia in the critically ill. Crit Care Clin 2004;20: 159–78.10.1016/j.ccc.2004.01.002Search in Google Scholar PubMed
2. von Ahsen N, Müller C, Serke S, Frei U, Eckardt KU. Important role of non diagnostic blood loss and blunted erythropoietic response in the anemia of medical intensive care patients. Crit Care Med 1999;27:2630–9.10.1097/00003246-199912000-00005Search in Google Scholar PubMed
3. Vincent JL, Baron JF, Reinhart K, Gattinoni L, Thijs L, Webb A, et al. Anemia and blood transfusion in critically ill patients. J Am Med Assoc 2002;288:1499–507.10.1001/jama.288.12.1499Search in Google Scholar PubMed
4. Page C, Retter A, Wyncoll D. Blood conservation devices in critical care: a narrative review. Ann Intensive Care 2013;3:14.10.1186/2110-5820-3-14Search in Google Scholar PubMed PubMed Central
5. Trinh TH, Fleury M, Leo-Kodeli S, Gauvain JB. Indicators of transfusion decision in acute geriatric ward with an exclusive emergency room recruitment. Transfus Clin Biol 2015;22:42–8.10.1016/j.tracli.2014.12.002Search in Google Scholar PubMed
6. International committee for standardization in hematology. Recommendations for haemoglobinometry in human blood. Br J Haematol 1967;13:71–5.10.1111/j.1365-2141.1967.tb00751.xSearch in Google Scholar PubMed
7. Lardi AM, Hirst C, Mortimer AJ, McCollum CN. Evaluation of the HemoCue for measuring intra-operative haemoglobin concentrations. A comparison with the Coulter Max-M. Anesthesia 1998;53:349–52.10.1046/j.1365-2044.1998.00328.xSearch in Google Scholar PubMed
8. Bland JM, Altman DG. Agreed statistics: measurement method comparison. Anesthesiology 2012;116:182.10.1097/ALN.0b013e31823d7784Search in Google Scholar PubMed
9. Dong X, Mendes de Leon C, Artz A, Tang Y, Shah R, Evans D. A population-based study of hemoglobin, race, and mortality in elderly persons. J Gerontol A Biol Sci Med Sci 2008;63: 873–8.10.1093/gerona/63.8.873Search in Google Scholar PubMed
10. Riessen R, Behmenburg M, Blumenstock G, Guenon D, Enkel S, Schäfer R, et al. A simple “blood-saving bundle” reduces diagnostic blood loss and the transfusion rate in mechanically ventilated patients. PLoS One 2015;10:e0138879.10.1371/journal.pone.0138879Search in Google Scholar PubMed PubMed Central
11. Lelubre C, Vincent JL. Red blood cell transfusion in the critically ill patient. Ann Intensive Care 2011;1:43.10.1186/2110-5820-1-43Search in Google Scholar PubMed PubMed Central
12. Myers GJ, Browne J. Point of care hematocrit and hemoglobin in cardiac surgery: a review. Perfusion 2007;22:179–83.10.1177/0267659107080826Search in Google Scholar PubMed
13. Gehring H, Hornberger C, Dıbbelt L, Rothsigkeit A, Gerlach K, Schumacher J, et al. Accuracy of point of care testing (POCT) for determining hemoglobin concentrations. Acta Anaesthesiol Scand 2002;46:980–6.10.1034/j.1399-6576.2002.460809.xSearch in Google Scholar PubMed
14. Seguin P, Kleiber A, Chanavaz C, Morcet J, Malledant Y. Determination of capillary hemoglobin levels in intensive care patients. J Crit Care 2011;26:423–7.10.1016/j.jcrc.2010.08.012Search in Google Scholar PubMed
15. Mimoz O, Frasca A, Medard A, Soubiron L, Debaene B, Dahyot-Fizelier C. Reliability of the HemoCue hemoglobinometer in critically ill patients: a prospective observational study. Minerva Anestesiol 2011;77:979–84.Search in Google Scholar PubMed
16. Van de Louw, Lassere N, Drouhin F, Thierry S, Lecuyer L, Caen D, et al. Reliability of HemoCue in patients with gastrointestinal bleeding. Intensive Care Med 2007;33:355–8.10.1007/s00134-006-0461-6Search in Google Scholar PubMed
17. Munoz M, Romero A, Gomez JF, Manteca A, Naveira E, Ramirez G. Utility of point of care haemoglobin measurement in the HemoCue-B haemoglobin for the initial diagnosis of anemia. Clin Lab Haemotol 2005;27:99–104.10.1111/j.1365-2257.2005.00678.xSearch in Google Scholar PubMed
18. Ripmann CE, Nett PC, Popovic D, Seifert B, Pasch T, Spahn DR. Hemocue, an accurate bedside method of hemoglobin measurement? J Clin Monit 1997;13:373–7.10.1023/A:1007451611748Search in Google Scholar PubMed
©2018 Walter de Gruyter GmbH, Berlin/Boston
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Articles in the same Issue
- Frontmatter
- Pediatric Laboratory Medicine
- Mucopolysaccharidosis VI diagnosis by laboratory methods
- Cord blood nucleated red blood cell level: is it a predictive marker for neonatal jaundice?
- Endocrinology
- Protein carbonylation in freshly diagnosed hypothyroidism is independent of thyrotropin levels
- Saliva and serum ghrelin and obestatin in iron deficiency anemia patients
- Point-of-Care-Testing
- The evaluation of point-of-care testing for determining hemoglobin levels in geriatric intensive care patients
- Neurology Laboratory
- Oxidative and nitrosative stress in patients with ischemic stroke
- Original Articles
- Validation of blood counters for quality control of platelet concentrates with high platelet counts
- Evaluation of the analytical performance of the Beckman Coulter Unicel DXI 800 Access Total 25(OH) Vitamin D immunoassay
- Laboratory Case Report
- Green urine – understanding its importance
Articles in the same Issue
- Frontmatter
- Pediatric Laboratory Medicine
- Mucopolysaccharidosis VI diagnosis by laboratory methods
- Cord blood nucleated red blood cell level: is it a predictive marker for neonatal jaundice?
- Endocrinology
- Protein carbonylation in freshly diagnosed hypothyroidism is independent of thyrotropin levels
- Saliva and serum ghrelin and obestatin in iron deficiency anemia patients
- Point-of-Care-Testing
- The evaluation of point-of-care testing for determining hemoglobin levels in geriatric intensive care patients
- Neurology Laboratory
- Oxidative and nitrosative stress in patients with ischemic stroke
- Original Articles
- Validation of blood counters for quality control of platelet concentrates with high platelet counts
- Evaluation of the analytical performance of the Beckman Coulter Unicel DXI 800 Access Total 25(OH) Vitamin D immunoassay
- Laboratory Case Report
- Green urine – understanding its importance

