Abstract
Objectives
To establish and verify the prediction model of recurrent preeclampsia (PE) in pregnant women with a history of PE.
Methods
Totally 130 pregnant women with a history of PE from Jan 2021 to Jan 2023 were selected retrospectively. The patients were randomly matched according to the proportion of 1:4 to establish a verification group (nasty 26) and a modeling group (nasty 104). The modeling patients were divided into two groups according to the occurrence of preeclampsia: recurrent group (nasty 50) and non-recurrent group (nasty 54). Multivariate logistic regression analysis of influencing factors was established. Calibration curve was performed to verify, decision curve analysis (DCA) was used to evaluate the clinical practicability of the prediction model, and ROC analysis was used to show the prediction value of the model.
Results
Multivariate logistic regression analysis showed that there were significant differences in age, gestational age, gestational interval, systolic blood pressure and diastolic blood pressure of previous pregnancy. (p<0.05) According to the results of logistic regression analysis, a prediction model was constructed. Logit(P)=(0.910Age)+(0.987Age of onset of previous pregnancy)+(1.167Gestational interval)+(1.186Systolic blood pressure in previous pregnancy)+(0.970Diastolic blood pressure in previous pregnancy).The slope of the calibration curve was close to one in the training set and verification set. The results showed that the prediction of recurrent PE risk of pregnant women with history of eclampsia was consistent with the actual risk. ROC analysis showed that the area under curve was 0.991. The results of DCA analysis showed that the model had good clinical practicability.
Conclusions
In this study, a prediction model is successfully established and verified according to the influencing factors.
Introduction
Preeclampsia (Pre-eclampsia), also known as preeclampsia, is a pregnancy-specific hypertensive disease, which usually occurs after 20 weeks of pregnancy, characterized by elevated blood pressure and proteinuria, which may be accompanied by damage to the function of other maternal organs [1], 2]. Unlike eclampsia, preeclampsia is the state of preeclampsia, which may develop into eclampsia without proper treatment. Recurrent preeclampsia is a serious complication of pregnancy, which is omni-directional and poses a serious threat to pregnant women and fetuses [3], [4], [5]. For pregnant women, recurrent preeclampsia may lead to cardiovascular system damage and increase the risk of cardiovascular disease; at the same time, it may lead to renal dysfunction and even renal failure; it may also cause liver function damage, abnormal blood coagulation and systemic edema [6]. These complications not only affect the health of pregnant women, but also lead to dangerous conditions during delivery, such as heart failure, pulmonary edema and so on [7], [8], [9], [10]. For the fetus, recurrent preeclampsia may lead to intrauterine hypoxia, affecting its normal growth and development. Due to impaired placental function, the fetus may be at risk of growth restriction, resulting in a lower body weight than normal at the same gestational age. In addition, recurrent preeclampsia may also increase the risk of premature delivery or stillbirth, posing a serious threat to the life and safety of the fetus [11]. In addition to direct hazards, recurrent preeclampsia may also have a long-term impact on the future health of pregnant women and fetuses [12], [13], [14]. For example, pregnant women may face a long-term risk of cardiovascular disease after preeclampsia, while fetuses affected by hypoxia and malnutrition may suffer irreversible damage to their nervous system, affecting their future cognitive and motor function. Previous studies by Wainstock et al. [15]. have shown that cesarean section and preterm labor are important risk factors for recurrent preeclampsia, but there is a lack of relevant research on model prediction that combines factors. The establishment of predictive models also aids in strengthening the self-management of pregnant women. By understanding the results of predictive models, pregnant women can gain a clearer understanding of their condition and risks, thereby more actively participating in prenatal care and disease prevention and enhancing their self-care awareness and capabilities [16], [17], [18]. Therefore, this study analyzes the factors influencing the recurrence of PE in pregnant women with a history of the condition and further establishes a predictive model to provide a reference for clinical practice.
Subjects and methods
Study subjects
In this retrospective study, we selected 130 cases of pregnant women with a history of preeclampsia who were admitted to our hospital from Jan 2021 to Jan 2023. The patients were randomly matched at a 1:4 ratio to establish a validation group (n=26) and a modeling group (n=104). Patients were divided into two groups based on the occurrence of preeclampsia: the recurrence group (n=50) and the non-recurrence group (n=54). The inclusion criteria were: (1) a history of only one prior delivery; (2) singleton pregnancy; (3) the same spouse for the pregnant woman; (4) no pharmacological prophylactic treatment used; (5) 18–35 years old. Exclusion criteria included: (1) pregnant women with primary cardiovascular disease; (2) those with hematologic disorders; (3) those with severe liver or kidney diseases; (4) suffering from gestational diabetes mellitus; (5) autoimmune diseases exist.
Data collection
Data collection included patients BMI, pregnancy-associated internal medical conditions, regular prenatal check-ups, conception method, HDL-C, LDL-C, urinary albumin-to-creatinine ratio (uACR), mode of delivery, age, gestational age at onset in the previous pregnancy, interpregnancy interval, and systolic and diastolic blood pressures during the previous pregnancy.
Diagnostic criteria for preeclampsia
Blood pressure criteria: In pregnant women after 20 weeks of gestation, SBP ≥140 mmHg and/or DBP >90 mmHg were considered high.
Proteinuria criteria: Accompanied by pro ≥0.3 g/24 h, or a positive result (+) in random urine protein tests.
Accompanying symptoms or signs: Typ: platelet count <100 × 109/L. Liver function impairment: serum transaminase levels more than twice the normal value. Kidney function impairment: SCR >97 μmol/L or more than twice the normal value. Pulmonary edema: clinical presentation of PE. New onset of central nervous system abnormalities or visual disturbances, such as headaches, blurred vision, or consciousness disturbances.
Statistical analysis
The collected experimental data were analyzed using SPSS version 27.0. Data fitting a normal distribution were expressed as mean ± standard deviation and compared using the independent sample t-test. Categorical data were expressed in numbers or percentages and compared using the chi-square test or Fisher’s exact test. Binary logistic regression analyses were conducted to identify factors influencing the recurrence of preeclampsia in pregnant women with a history of the condition. The predictive value of the model for recurrence in these women was assessed using the receiver operating characteristic curve (ROC), calibration curve was performed to verify, decision curve analysis (DCA) was used to evaluate the clinical practicability of the prediction model. p<0.05 were generally considered as statistically significant.
Results
Comparison of general data
The comparison of general data between the validation group and the modeling group showed no differences (p>0.05), as shown in Table 1.
Comparison of general data.
| Indicator | Validation group (n=26) | Modeling group (n=104) | t/χ2 value | p-Value | |
|---|---|---|---|---|---|
| Age, years | 28.45 ± 2.45 | 28.62 ± 2.33 | 0.329 | 0.742 | |
| BMI, kg/m2 | 21.48 ± 2.37 | 21.73 ± 2.14 | 0.521 | 0.603 | |
| Age of onset of previous pregnancy, w | <28 | 5 | 23 | 0.510 | 0.917 |
| 28∼34 | 13 | 56 | |||
| >34 | 8 | 25 | |||
| Gestational interval, years | <5 | 15 | 51 | 0.623 | 0.732 |
| ≥5 | 11 | 53 | |||
| Pregnancy complicated with medical diseases | Yes | 6 | 21 | 0.105 | 0.949 |
| N/A | 20 | 83 | |||
| Regular prenatal examination during pregnancy | Yes | 10 | 46 | 0.282 | 0.868 |
| N/A | 16 | 58 | |||
| Mode of conception | Natural | 25 | 101 | – | 1.000 |
| IVF | 1 | 3 | |||
| HDL-C, mmol/L | 1.30 ± 0.13 | 1.28 ± 0.19 | 0.507 | 0.613 | |
| LDL-C, mmol/L | 2.76 ± 0.31 | 2.71 ± 0.29 | 0.776 | 0.439 | |
| uACR | 3.32 ± 0.11 | 3.36 ± 0.29 | 0.689 | 0.492 | |
| Mode of delivery | Natural delivery | 3 | 13 | – | 1.000 |
| Cesarean section | 23 | 91 | |||
| Systolic blood pressure in previous pregnancy, mmHg | <160 | 14 | 55 | 0.007 | 0.996 |
| ≥160 | 12 | 49 | |||
| Diastolic blood pressure in previous pregnancy, mmHg | <110 | 16 | 66 | 0.033 | 0.984 |
| ≥110 | 10 | 38 |
Comparison of two sets of baseline data
Analysis indicated that there were no significant differences in BMI, pregnancy-associated internal medical conditions, regularity of prenatal check-ups, conception method, significant differences were found in age (t=5.208, p<0.001), gestational age at onset in the previous pregnancy (t=17.061, p<0.001), interpregnancy interval (χ2=8.625, p=0.013), systolic blood pressure in previous pregnancy (χ2=6.416, p=0.040), diastolic blood pressure in previous pregnancy (χ2=9.051, p=0.011). It is suggested that age, gestational age, gestational interval, systolic blood pressure and diastolic blood pressure may be the influencing factors of recurrent preeclampsia. as shown in Table 2.
Comparison of two sets of baseline data.
| Indicator | Recurrence group (n=50) | Non-recurrence group (n=54) | t/χ2 value | p-Value | |
|---|---|---|---|---|---|
| Age, years | 30.15 ± 2.44 | 27.77 ± 2.22 | 5.208 | <0.001 | |
| BMI, kg/m2 | 21.55 ± 2.43 | 21.67 ± 2.37 | 0.255 | 0.799 | |
| Age of onset of previous pregnancy, w | <28 | 19 | 4 | 17.061 | 0.001 |
| 28∼34 | 25 | 31 | |||
| >34 | 6 | 19 | |||
| Gestational interval, years | <5 | 32 | 19 | 8.625 | 0.013 |
| ≥5 | 18 | 35 | |||
| Pregnancy complicated with medical diseases | Yes | 10 | 11 | 0.002 | 0.999 |
| N/A | 40 | 43 | |||
| Regular prenatal examination during pregnancy | Yes | 22 | 24 | 0.002 | 0.999 |
| N/A | 28 | 30 | |||
| Mode of conception | Natural | 49 | 52 | – | 1.000 |
| IVF | 1 | 2 | |||
| HDL-C, mmol/L | 1.28 ± 0.23 | 1.27 ± 0.28 | 0.198 | 0.843 | |
| LDL-C, mmol/L | 2.70 ± 0.52 | 2.72 ± 0.51 | 0.198 | 0.843 | |
| uACR | 3.35 ± 0.24 | 3.37 ± 0.37 | 0.324 | 0.746 | |
| Mode of delivery | Natural delivery | 6 | 8 | – | 0.781 |
| Cesarean section | 42 | 46 | |||
| Systolic blood pressure in previous pregnancy, mmHg | <160 | 20 | 35 | 6.416 | 0.040 |
| ≥160 | 30 | 19 | |||
| Diastolic blood pressure in previous pregnancy, mmHg | <110 | 27 | 44 | 9.051 | 0.011 |
| ≥110 | 23 | 10 |
Multivariable analysis
Using age, gestational age at onset during the previous pregnancy, interpregnancy interval, and systolic and diastolic pressures from the previous pregnancy as independent variables, and the outcome of eclampsia recurrence (recurrent eclampsia=1, no recurrence=0) as the dependent variable. The results showed that age (OR=3.165, 95 % CI=1.352–7.410), age of onset of previous pregnancy (OR=2.915, 95 % CI=1.336–6.360), gestational interval (OR=2.864, 95 % CI=1.088–7.542), systolic blood pressure (OR=3.154, 95 % CI=1.090–9.125) and diastolic blood pressure of previous pregnancy (OR=3.284, 95 % CI=1.160–9.298) were independent influencing factors of recurrent preeclampsia in pregnant women with history of PE.as indicated in Table 3.
Multivariable analysis.
| Influencing factors | β value | SE value | WALD | p-Value | Exp, B | 95%CI | |
|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||
| Age | 0.910 | 0.370 | 7.042 | 0.008 | 2.483 | 1.202 | 5.129 |
| Age of onset of previous pregnancy | 0.987 | 0.243 | 17.207 | <0.001 | 2.529 | 1.630 | 10.913 |
| Gestational interval | 1.167 | 0.477 | 5.784 | 0.010 | 3.195 | 1.262 | 8.172 |
| Systolic blood pressure in previous pregnancy | 1.186 | 0.640 | 3.439 | 0.040 | 3.228 | 1.935 | 9.468 |
| Diastolic blood pressure in previous pregnancy | 0.970 | 0.382 | 5.993 | 0.024 | 2.545 | 1.244 | 5.640 |
Development of a predictive model
Based on the results of the logistic regression analysis, age, gestational age at onset during the previous pregnancy, interpregnancy interval, and blood pressures from the previous pregnancy were incorporated into a model predicting the recurrence of preeclampsia in pregnant women with a history of the condition. The model formula is Logit(P)=(0.910Age)+(0.987Age of onset of previous pregnancy)+(1.167Gestational interval)+(1.186Systolic blood pressure in previous pregnancy)+(0.970Diastolic blood pressure in previous pregnancy). The clinical benefits are shown in Figure 1. The results of DCA analysis showed that the model had good clinical practicability. The model curve demonstrates superior performance by being positioned closer to the upper right corner compared to the curve representing all interventions (ALL), suggesting that interventions guided by the model yield greater benefits than blanket interventions across the board, as illustrated in Figure 1. To construct the calibration curve, the prediction probabilities are categorized into distinct buckets, employing either a ‘uniform’ or ‘quantile’ division strategy. Within each bucket, the average prediction probability of all samples is computed and designated as the abscissa (x-axis). Concurrently, the probability of positive instances within the same bucket is calculated and assigned as the ordinate (y-axis). By sequentially connecting these calculated points, the calibration curve is effectively plotted, providing a visual representation of the model’s predictive accuracy. This model showed calibration curves with slopes close to 1 in both the training and validation sets, indicating good consistency between the predicted risks and the actual risks, as shown in Figures 2 and 3.
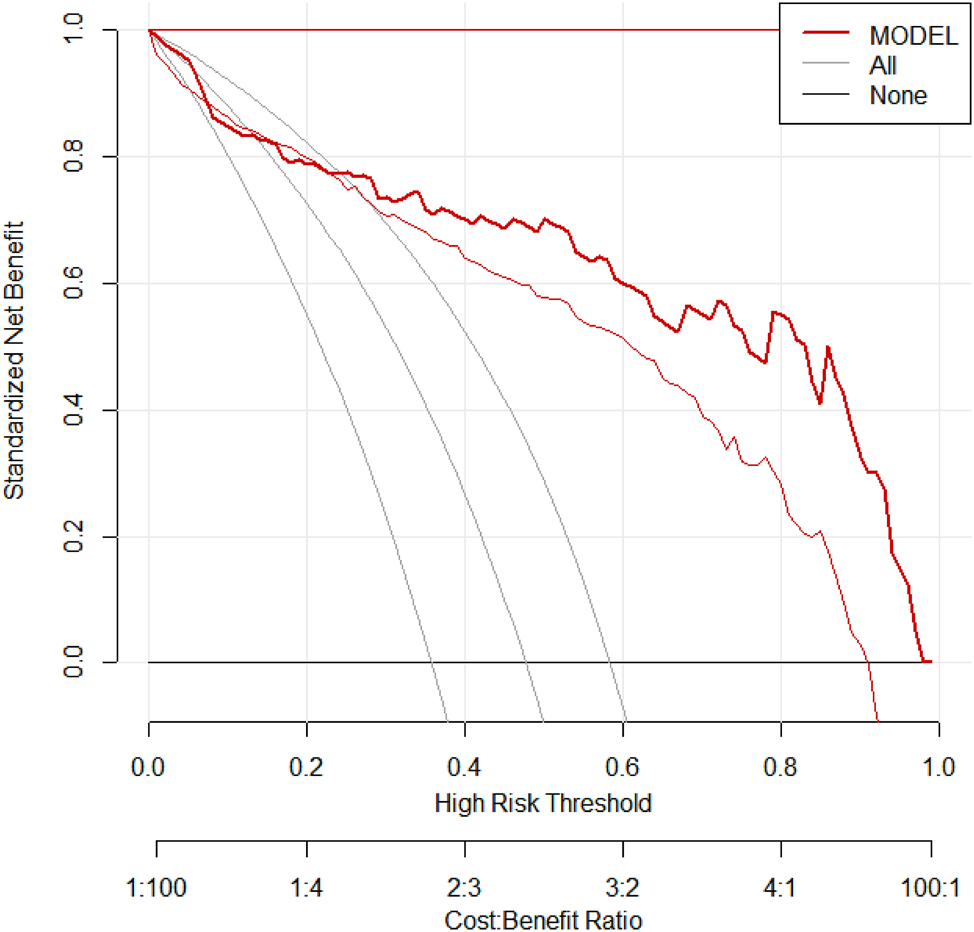
Predictive model. Note: Successful establishment of prediction model.
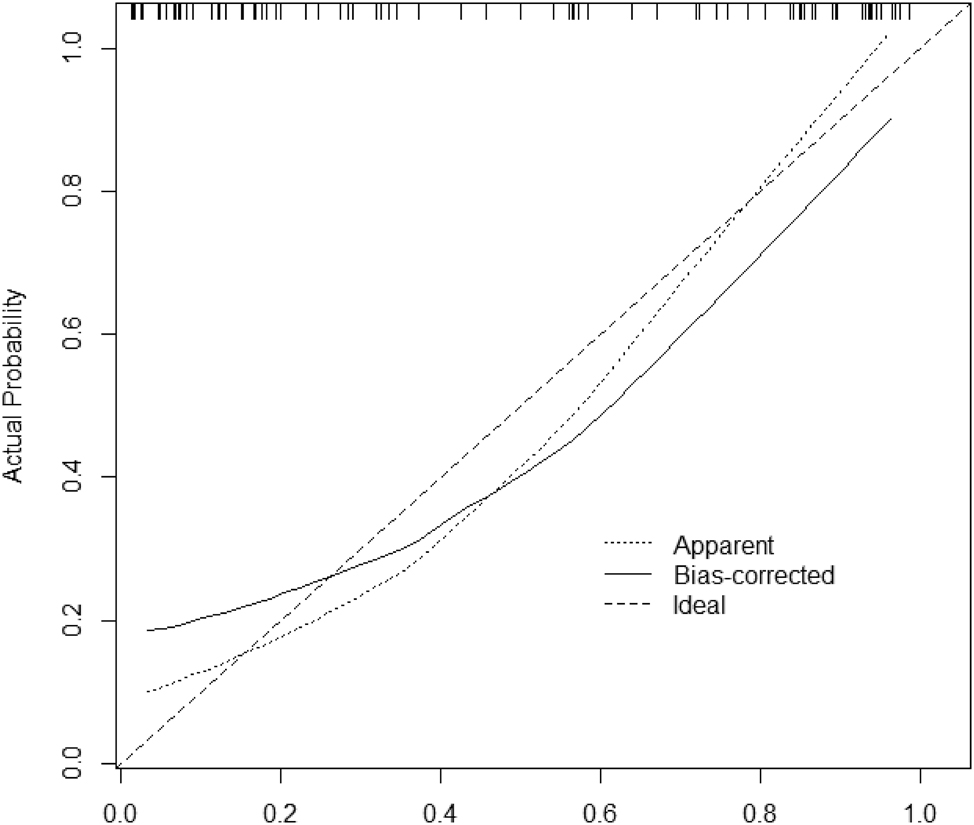
Training set calibration curve. Note: The slope of the calibration curve is close to 1, indicating that the risk is in good agreement with the actual risk.
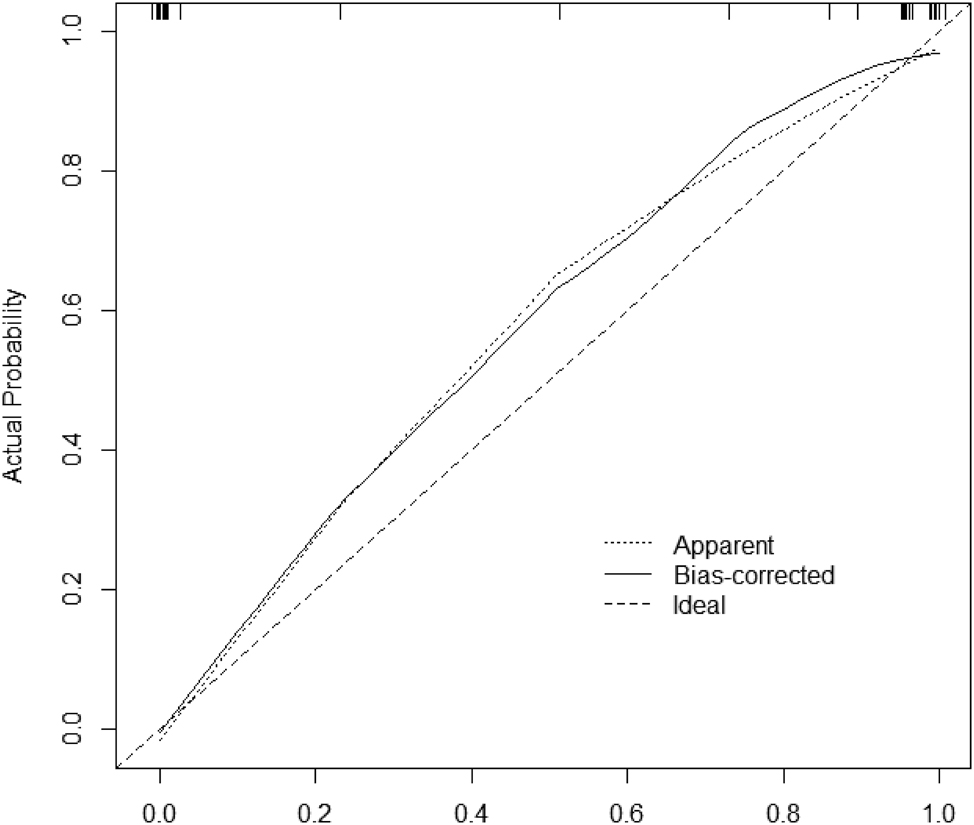
Validation set calibration curve. Note: The slope of the calibration curve is close to 1, indicating that the risk is in good agreement with the actual risk.
ROC curve analysis of the predictive model’s value in forecasting recurrence of preeclampsia in pregnant women with a history of preeclampsia
ROC analysis demonstrated that in the training set, the AUC for predicting the recurrence of preeclampsia in pregnant women with a history of the condition was 0.898 with a standard error of 0.034 as shown in Figure 4. In the validation set, the AUC was 0.991 with a standard error of 0.001 as shown in Figure 5.
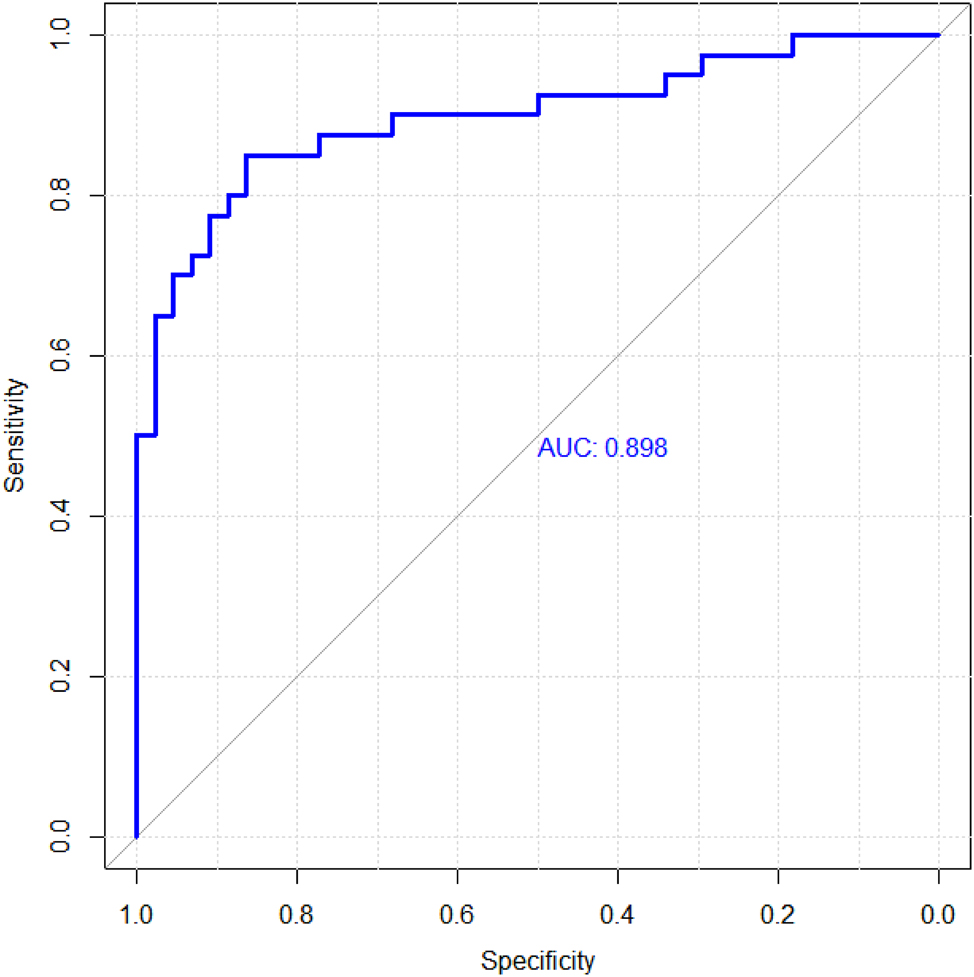
Training set roc curve. Note: The area under the ROC curve is approximately one, indicating that the prediction value is good.
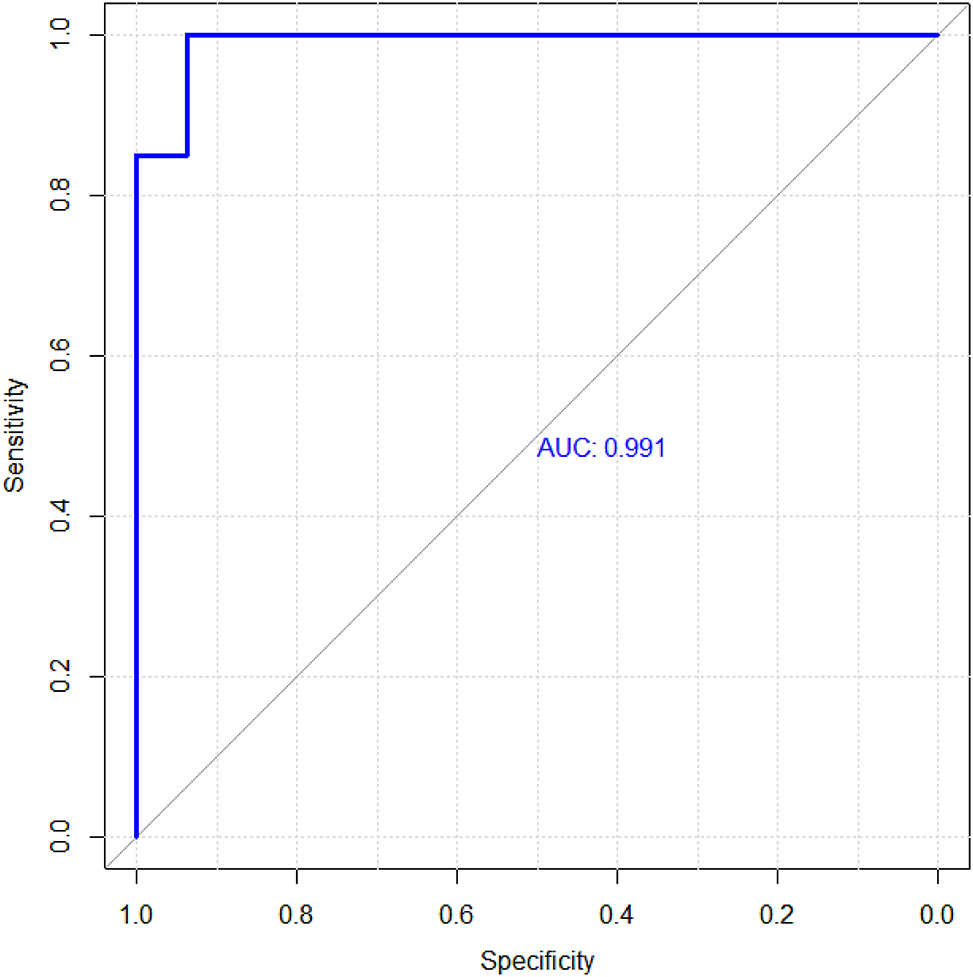
Validation set ROC curve. Note: The area under the ROC curve is approximately one, indicating that the prediction value is good.
Discussion
The risk of recurrence of preeclampsia increases significantly during second pregnancy, which poses a great threat to maternal and infant health. Therefore, to explore the influencing factors of its recurrence and establish an effective prediction model is of great significance to improve the quality of pregnancy management and reduce the risk of maternal and infant complications [19], 20]. In this study, by comparing the general data of patients in the verification group and the model group, and the results of this study, to explore the influencing factors of recurrence, and based on these factors to build a predictive model, and then verify.
The results showed that there were statistically significant differences between patients in the Recurrence group and Non-recurrence group in age, gestational week starting during the previous pregnancy, pregnancy interval, systolic blood pressure during the previous pregnancy, and systolic blood pressure during the previous pregnancy (p<0.05). Multivariate logistic results further demonstrated that these factors are independent influencing factors on recurrence. One possible explanation for these findings is that as women age, their physiological functions gradually decline and the elasticity of their blood vessels decreases, potentially leading to reduced adaptability to hypertension during pregnancy [21], [22], [23]. Additionally, aging is associated with an increased risk of various chronic diseases, which may further impact blood pressure control during pregnancy [24], 25]. Earlier onset of disease in a previous pregnancy may indicate more severe impairment of endothelial function in pregnant women, or the presence of some yet unidentified genetic factors or pathophysiological processes [26], [27], [28]. These factors could be reactivated during a subsequent pregnancy, leading to an earlier or more severe onset of preeclampsia. A shorter inter-pregnancy interval (less than 5 years) may affect a woman’s physical recovery and adaptability. A short interval might mean the body has not fully recovered before becoming pregnant again, with previous pregnancy blood pressure levels directly reflecting the woman’s blood pressure condition [29], [30], [31]. Higher blood pressure levels may indicate some degree of vascular dysfunction or damage, which could persist or worsen in a subsequent pregnancy, leading to the recurrence of preeclampsia.
This study constructed a mode (Logit(P)=(0.910Age)+(0.987Age of onset of previous pregnancy)+(1.167Gestational interval)+(1.186Systolic blood pressure in previous pregnancy)+(0.970Diastolic blood pressure in previous pregnancy) l to predict the risk of recurrent PE in pregnant women with a history of PE.The model included age, gestational age, gestational interval, systolic blood pressure and diastolic blood pressure of previous pregnancy as predictive factors.The results of the study show that women with advanced age, shorter gestational weeks after the onset of previous pregnancies, shorter pregnancy intervals, and higher systolic and diastolic blood pressures in previous pregnancies are at greater risk. The model built in this study inputs data such as age, age of onset of first pregnancy, pregnancy interval, systolic and diastolic blood pressure of previous pregnancies, and the algorithm can calculate the probability of recurrence risk. For example, a 35-year-old pregnant woman with a first pregnancy of 28 years, a pregnancy interval of 2 years, and a previous pregnancy with a systolic blood pressure of 150 mmHg and a diastolic blood pressure of 100 mmHg, put the data into the model. The result is that at 337, the risk threshold indicates that she has a high risk of recurrent PE. Doctors can add preventive measures in advance to reduce the probability of recurrence.The performance evaluation of the model shows that the slope of the calibration curve is close to 1 in both the training set and the verification set, which strongly indicates that there is a good consistency between the risk predicted by the model and the actual observed risk. In the training set, the results of ROC analysis showed that AUC of the model for predicting recurrent preeclampsia was 0.898, and the standard error was 0.034 When the optimal truncation value is set to 0.85, the sensitivity of the model is 93.4 % and the specificity is 91.1 %, indicating that the model has high accuracy in identifying pregnant women who will actually have preeclampsia again. At the same time, the proportion of women who mistakenly identify low-risk pregnant women as high-risk is also relatively low. In the verification set, the performance of the model is further verified. ROC analysis results show that the AUC is as high as 0.991 and the standard error is 0.001. When the optimal truncation value is 0.94, the sensitivity of the model is 93.5 %, and the specificity is 100.0 %. The prediction model based on Logistic regression shows good accuracy and reliability in predicting the risk of recurrent PE in pregnant women with a history of preeclampsia. It provides clinicians and pregnant women with a powerful tool to assess and manage the risk of second pregnancy.
Limitation
Although this study has made some achievements in predicting the risk of This time the researchers, there are still some shortcomings. First, the size and diversity of the sample could be limiting factors. Although an adequate number of samples were collected as much as possible, a larger sample size might provide more representative and stable results. Additionally, the diversity of the sample may affect the generalizability of the model, that is, the model’s predictive effectiveness across different populations. Furthermore, the validation and evaluation of the model also face challenges. While this study used training and validation sets to assess the model’s performance, more external datasets and real-world application scenarios might reveal limitations and deficiencies of the model in practical use. Future research should aim to expand the sample size, consider more potential influencing factors, and explore more advanced predictive models and methods to enhance prediction accuracy and stability.
Conclusions
To sum up, this study provides new ideas and tools for predicting, preventing and controlling the recurrence of preeclampsia in pregnant women with a history of preeclampsia. Through further research and practice, the predictive model is combined with clinical practice to give full play to its value.
Acknowledgments
The authors are grateful to all participants in the present study.
-
Research ethics: This study protocol was reviewed and approved by the Ethics Committee of Tianjin Central Hospital of Gynecology Obstetrics in accordance with regulatory and ethical guidelines (2020KY122).
-
Informed consent: Informed consent was waived for this retrospective study due to the exclusive use of de-identified patient data, which posed no potential harm or impact on patient care.
-
Author contributions: All authors contributed to the study conception and design. Material preparation, data collection and analysis was performed by HD, JS and XC. The first draft of the manuscript was written by HD, JS and YJJ. HYC and XC commented on previous versions of the manuscript. All authors read and approved the final manuscript.
-
Use of Large Language Models, AI and Machine Learning Tools: This study did not use of large language models, AI and machine learning tools.
-
Conflict of interest: The authors declare that they have no conflict of interest.
-
Research funding: This study did not receive any form of funding.
-
Data availability: The data involved in the present study can be provided under reasonable request.
References
1. Ismailova, I, Zame, Y, Akhmedzhanova, M, Sultanov, K, Tanzharykova, G. Pathogenetic role of a number of factors in the development and progression of preeclampsia with varying severity in pregnant women. Reprod Fertil Dev 2024;36. https://doi.org/10.1071/rd23214.Search in Google Scholar
2. Ito, T, Takahashi, H, Horie, K, Nagayama, S, Ogoyama, M, Fujiwara, H. Confined placental mosaicism with trisomy 13 complicated by severe preeclampsia: a case report and literature review. J Obstet Gynaecol Res 2024;50:1737–41. https://doi.org/10.1111/jog.16035.Search in Google Scholar PubMed
3. Jiang, H, Meng, T, Li, Z. Role of circular RNAs in preeclampsia (Review). Exp Ther Med 2024;28:372. https://doi.org/10.3892/etm.2024.12661.Search in Google Scholar PubMed PubMed Central
4. Lundgaard, MH, Sinding, MM, Sorensen, AN, Handberg, A, Andersen, S, Andersen, SL. Maternal hypothyroidism and the risk of preeclampsia: a Danish national and regional study. Matern Health Neonatol Perinatol 2024;10:16. https://doi.org/10.1186/s40748-024-00186-4.Search in Google Scholar PubMed PubMed Central
5. Sligo, J, Corfe-Tan, J, Cotter, Z, Eteuati, JS, Hart, HR, McConnell, R. Midwifery experiences in rural Southern Aotearoa New Zealand: insights into pre-eclampsia management. N Z Med J 2024;137:52–61. https://doi.org/10.26635/6965.6458.Search in Google Scholar PubMed
6. Saffian, E, Palatnik, A. Association between recurrent preeclampsia and attendance at the blood pressure monitoring appointment after birth. J Obstet Gynecol Neonatal Nurs 2024;53:132–9. https://doi.org/10.1016/j.jogn.2023.11.002.Search in Google Scholar PubMed PubMed Central
7. Han, S, Zhang, H, He, Y, Chen, Q. Clinical features of recurrent preeclampsia: a retrospective study of 109 recurrent preeclampsia patients. Hypertens Res 2024;47:1410–9. https://doi.org/10.1038/s41440-024-01623-9.Search in Google Scholar PubMed
8. Tulin Gesoglu, D, Murat, C, Dilek, A, Ozlem, E, Sibel, S. Risk factors of posterior reversible encephalopathy syndrome in patients with preeclampsia or eclampsia: a retrospective review. Ideggyogy Sz 2024;77:247–54. https://doi.org/10.18071/isz.77.0247.Search in Google Scholar PubMed
9. Wu, C, Ling, Z, Wang, Y, Lv, Y, Miao, Z, Liu, L, et al.. Clinical analysis of risk factors and perinatal outcomes in recurrent pre-eclampsia with severe features. Reprod Sci 2024;31:2763–70. https://doi.org/10.1007/s43032-024-015294.Search in Google Scholar
10. Zhang, L, Wang, W, Gong, J, Wang, X, Liang, J, Gu, S, et al.. Development, validation, and clinical utility of a risk prediction model for recurrent preeclampsia. J Hypertens 2024;42:236–43. https://doi.org/10.1097/hjh.0000000000003580.Search in Google Scholar
11. Stanciakova, L, Dobrotova, M, Ivankova, J, Skornova, I, Bolek, T, Brunclikova, M, et al.. At-risk pregnant woman with sticky platelet syndrome, previous recurrent preeclampsia, and current proteinuria - a rare experience. Rev Invest Clin 2023;75:45–6. https://doi.org/10.24875/RIC.22000307.Search in Google Scholar PubMed
12. Bijl, RC, Cornette, JMJ, Brewer, AN, Zwart, IF, Franx, A, Tsigas, EZ, et al.. Patient-reported preconceptional characteristics in the prediction of recurrent preeclampsia. Pregnancy Hypertens 2022;28:44–50. https://doi.org/10.1016/j.preghy.2022.02.003.Search in Google Scholar PubMed
13. Lin, XM, Li, DZ. Prevention of recurrent preeclampsia in high-risk pregnancies: is it time for a paradigm shift? Am J Obstet Gynecol 2023;229:187–8. https://doi.org/10.1016/j.ajog.2023.03.035.Search in Google Scholar PubMed
14. Ma, Y, Ma, M, Ye, S, Liu, Y, Zhao, X, Wang, Y. Association of IL-17 and IL-27 polymorphisms with susceptibility to recurrent pregnancy loss and pre-eclampsia: a systematic review and meta-analysis. Immun Inflamm Dis 2023;11:e1057. https://doi.org/10.1002/iid3.1057.Search in Google Scholar PubMed PubMed Central
15. Wainstock, T, Sheiner, E. Clinical factors associated with preeclampsia recurrence. Pregnancy Hypertens 2022;30:31–5. https://doi.org/10.1016/j.preghy.2022.08.004.Search in Google Scholar PubMed
16. de Moreuil, C, Alavi, Z, Pasquier, E. Hydroxychloroquine may be beneficial in preeclampsia and recurrent miscarriage. Br J Clin Pharmacol 2020;86:39–49. https://doi.org/10.1111/bcp.14131.Search in Google Scholar PubMed PubMed Central
17. Stekkinger, E, Scholten, RR, Heidema, WM, Spaanderman, MEA. Comparison of three definitions of metabolic syndrome and relation to risk of recurrent preeclampsia. Hypertens Pregnancy 2021;40:97–108. https://doi.org/10.1080/10641955.2021.1872614.Search in Google Scholar PubMed
18. Zhang, Y, Shen, F, Yang, W, Wang, J, Zhou, J, Chen, Y. Effects of low-molecular-weight heparin and aspirin in recurrent pre-eclampsia: a stratified cohort study. Int J Gynaecol Obstet 2021;154:337–42. https://doi.org/10.1002/ijgo.13535.Search in Google Scholar PubMed
19. Njoroge, S, Kuriloff, M, Mueller, A, Lopes Perdigao, J, Dhir, R, Rana, S. The interval between births and the risk of recurrent preeclampsia among predominantly high risk women in urban tertiary care center. Pregnancy Hypertens 2021;25:7–11. https://doi.org/10.1016/j.preghy.2021.05.009.Search in Google Scholar PubMed
20. Mulder, EG, Ghossein-Doha, C, Cauffman, E, Lopes van Balen, VA, Schiffer, V, Alers, RJ, et al.. Preventing recurrent preeclampsia by tailored treatment of nonphysiologic hemodynamic adjustments to pregnancy. Hypertension 2021;77:2045–53. https://doi.org/10.1161/hypertensionaha.120.16502.Search in Google Scholar PubMed
21. Dong, X, Han, M, Zeb, S, Tong, M, Li, X, Chen, Q. Active management reduces the incidence of recurrent pre-eclampsia and improves maternal and fetal outcomes in women with recurrent pre-eclampsia. Front Med 2021;8:658022. https://doi.org/10.3389/fmed.2021.658022.Search in Google Scholar PubMed PubMed Central
22. Yu, Z, Zhang, W, Wang, Y, Gao, M, Zhang, M, Yao, D, et al.. Extracellular vesicles derived from human umbilical cord MSC improve vascular endothelial function in in vitro and in vivo models of preeclampsia through activating arginine metabolism. Mol Pharm 2023;20:6429–40. https://doi.org/10.1021/acs.molpharmaceut.3c00816.Search in Google Scholar PubMed PubMed Central
23. Yang, X, Benny, PA, Cervera-Marzal, E, Wu, B, Lassiter, CB, Astern, J, et al.. Placental telomere length shortening is not associated with severe preeclampsia but the gestational age. Aging (Albany NY) 2022;15:353–70. https://doi.org/10.18632/aging.204445.Search in Google Scholar PubMed PubMed Central
24. Shi, J, Wang, J, Jia, N, Sun, Q. A network pharmacology study on mechanism of resveratrol in treating preeclampsia via regulation of AGE-RAGE and HIF-1 signalling pathways. Front Endocrinol 2022;13:1044775. https://doi.org/10.3389/fendo.2022.1044775.Search in Google Scholar PubMed PubMed Central
25. Mula, R, Prats, P, Garcia, S, Serra, B, Scazzocchio, E, Meler, E. Angiogenic factors assessment in pre-eclampsia high-risk population for the prediction of small-for-gestational age neonates: a prospective longitudinal study. Int J Gynaecol Obstet 2023;161:439–46. https://doi.org/10.1002/ijgo.14508.Search in Google Scholar PubMed
26. Liu, Y, Zhou, M, Cheng, H, Du, J. Effect of low-molecular-weight heparin calcium combined with magnesium sulfate and labetalol on coagulation, vascular endothelial function and pregnancy outcome in early-onset severe preeclampsia. Eur J Clin Pharmacol 2024;80:1495–501. https://doi.org/10.1007/s00228-024-03712-7.Search in Google Scholar PubMed
27. Deng, P, Yu, Q, Tang, H, Lu, Y, He, Y. Age at menarche mediating visceral adipose tissue’s influence on pre-eclampsia: a mendelian randomization study. J Clin Endocrinol Metab 2023;108:405–13. https://doi.org/10.1210/clinem/dgac566.Search in Google Scholar PubMed PubMed Central
28. Chen, Z, Wu, M, Huang, H, Tao, H, Zou, L, Luo, Q. Correction: plasma exosomal miR-199a-5p derived from preeclampsia with severe features impairs endothelial cell function via targeting SIRT1. Reprod Sci 2024;31:579. https://doi.org/10.1007/s43032-023-01416-4.Search in Google Scholar PubMed
29. Deng, Y, She, L, Li, X, Lai, W, Yu, L, Zhang, W, et al.. Monitoring hypertensive disorders in pregnancy to prevent preeclampsia in pregnant women of advanced maternal age: trial mimicking with retrospective data. Open Med 2022;17:1840–8. https://doi.org/10.1515/med-2022-0560.Search in Google Scholar PubMed PubMed Central
30. Yan, W, Zhou, Y. The application effect of evidence-based targeted nursing in severe preeclamptic women and its impact on maternal psychological status, uality of life, and maternal-infant outcomes. Altern Ther Health Med 2025;31:414–21.Search in Google Scholar
31. Jasper, EA, Hellwege, JN, Breeyear, JH, Xiao, B, Jarvik, GP, Stanaway, IB, et al.. Genetic predictors of blood pressure traits are associated with preeclampsia. Sci Rep 2024;14:17613. https://doi.org/10.1038/s41598-024-68469-6.Search in Google Scholar PubMed PubMed Central
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.

