Effectiveness of osteopathic manual treatment in the elderly population: a scoping review of clinical evidence
-
Livio Molinari
Abstract
Context
Osteopathic manipulative treatment (OMT) is an emerging nonpharmacological intervention utilized to address various health conditions, particularly among the elderly population. This scoping review aims to examine the available evidence regarding the effectiveness of OMT in improving pain, balance, and quality of life in geriatric patients, identifying gaps in the current research and suggesting future directions.
Objectives
This scoping review aims to evaluate the efficacy of OMT in elderly patients by analyzing selected studies that specifically explore its effects on balance, quality of life, and pain management. Additionally, this review will assess the current quality of evidence regarding these outcomes.
Methods
Selected articles from December 2012 to September 2024 focused on OMT in individuals aged 65 and older. We conducted a systematic literature search utilizing Medical Subject Headings (MeSH) and free-text terms combined with the Boolean operator “AND,” including: OMT, osteopathic manipulative treatment, osteopathic medicine, aging, older adult, elderly, aged, and geriatric people. Databases, including PubMed, SCOPUS, Cochrane Library, and others, were searched from June 3, 2024 to September 3, 2024 following Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines. Three authors (L.M., E.N., L.M.) reviewed the titles, abstracts, and full texts to determine eligibility. Disagreements were resolved through discussion. Filters included studies involving human subjects and studies published in English, Spanish, or Italian. Exclusions were made for literature reviews, protocols, commentaries, and nonosteopathic manual techniques.
Results
A total of 2,478 articles were identified; then, after removing 1,564 duplicates, 917 articles remained for screening. These articles were assessed based on their titles and abstracts, leading to the exclusion of 873 articles according to the established exclusion criteria. In the final phase, the remaining 44 articles underwent a full-text evaluation. This process resulted in the exclusion of 21 articles that were not randomized controlled trials (RCTs) and 14 articles that did not meet the required outcome measures. Ultimately, a total of nine articles were included in the systematic review.
Conclusions
This study highlights the effectiveness of OMT in improving pain, balance, and quality of life in geriatric patients. The findings underscore the value of OMT as a personalized therapeutic approach, promoting healthier aging and enhancing overall well-being in the elderly population. Further research is encouraged to explore the full potential of OMT, supporting its integration as a key component of osteopathic care for geriatric patients.
The aging of the population is a global phenomenon, with a steady increase in the number of people over the age of 65. The World Health Organization (WHO) estimates that by 2050, 22 % of the global population will be elderly, which will lead to an increased prevalence of chronic conditions such as musculoskeletal pain, osteoarthritis, and reduced mobility [1], 2]. With advancing age, musculoskeletal and systemic diseases become increasingly prevalent, significantly affecting quality of life among older adults. Common conditions include osteoarthritis and osteoporosis, affecting approximately 40 and 25 % of individuals over 65, respectively [3], 4]. Diabetes and cardiovascular disease, with prevalence rates of 30% and 40 %, further reduce functional independence and increase complication risks [5], 6]. Additionally, chronic obstructive pulmonary disease (COPD) impacts approximately 10 % of elderly individuals, compromising respiratory capacity and quality of life [7].
In this context, osteopathic manipulative treatment (OMT) has gained attention as a nonpharmacological intervention to improve quality of life and reduce pain in older adults [8], 9].
OMT consists of manual techniques designed to enhance joint mobility, soft tissue function, and circulation, thereby helping to alleviate pain and promote overall physical well-being [10], 11]. Several studies have explored the potential benefits of OMT in the elderly, indicating positive effects on chronic pain, mobility, and quality of life [12], 13]. For instance, research has shown that OMT can reduce musculoskeletal pain and improve motor function in elderly patients with osteoarthritis [10], as well as in those suffering from Pisa syndrome, a condition often associated with Parkinson’s disease [14].
In addition to OMT, other holistic medicine techniques and manual therapies, such as physical therapy, chiropractic care, and craniosacral therapy, have demonstrated promising benefits for the elderly population. Physical therapy, in particular, is commonly utilized to improve mobility and functionality, with studies showing that personalized exercise programs can reduce the risk of falls and enhance muscle strength in older adults [15], 16]. Chiropractic care has proven effective in treating lower back pain and neck pain, with evidence supporting spinal adjustments to improve functionality and alleviate pain [17], 18].
Moreover, craniosacral therapy, which focuses on the fluids and membranes of the central nervous system, has been studied for its potential to reduce pain and improve the quality of life in elderly patients with fibromyalgia and other chronic conditions [19]. Additionally, traditional Chinese medicine, including techniques such as acupuncture, has shown efficacy in reducing pain and improving mobility in older adults, helping to manage conditions like arthritis and carpal tunnel syndrome [20].
Despite these promising findings, the current literature has several limitations. Small sample sizes, a lack of adequate control groups, and variability in the techniques utilized restrict the generalizability of the results [11], [12], [13], [14], [15]. Furthermore, long-term follow-up studies are needed to assess the durability of OMT’s benefits and to better understand its underlying mechanisms [12], 13].
This scoping review aims to map the existing evidence on the effectiveness of OMT and other holistic medicine techniques in the elderly population, identifying reported benefits and areas where further research is needed. The objective is to provide a comprehensive overview of current scientific findings and contribute to the development of future clinical guidelines.
Methods
Study selection
For our review, all articles published online that focus on OMT in the elderly population, between December 2012 and September 2024, were considered. The time frame for the bibliographic search of the randomized controlled trials (RCTs) was conducted between June 3, 2024, and September 3, 2024. The authors who conducted the bibliographic search were L.M., L.M., and E.N., without any disagreement during this research phase.
The title, abstract, and full text of each study were examined by three authors (L.M., L.M., E.N.) to evaluate potentially eligible studies. Initially selected based on the title and abstract, the studies were subsequently included after further screening through the full text. In cases of uncertainty (e.g., no available abstract or unclear details), the full article was reviewed. The selected articles were collected in a database and screened for relevance. Any disagreement between the authors was resolved through discussion and alignment on the eligibility of each article.
Protocol and registration
Although a formal protocol was not published, the exploratory nature of this review and the limited research available in this domain required a strong emphasis on methodological rigor and reproducibility. This was accomplished by strictly following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines [21].
Eligibility criteria
All experimental articles (RCTs, systematic reviews, meta-analyses, case reports, and case series) were initially selected. Subsequently, for this review, only RCT articles were considered, utilizing the PRISMA (Figure 1) process for literature selection.
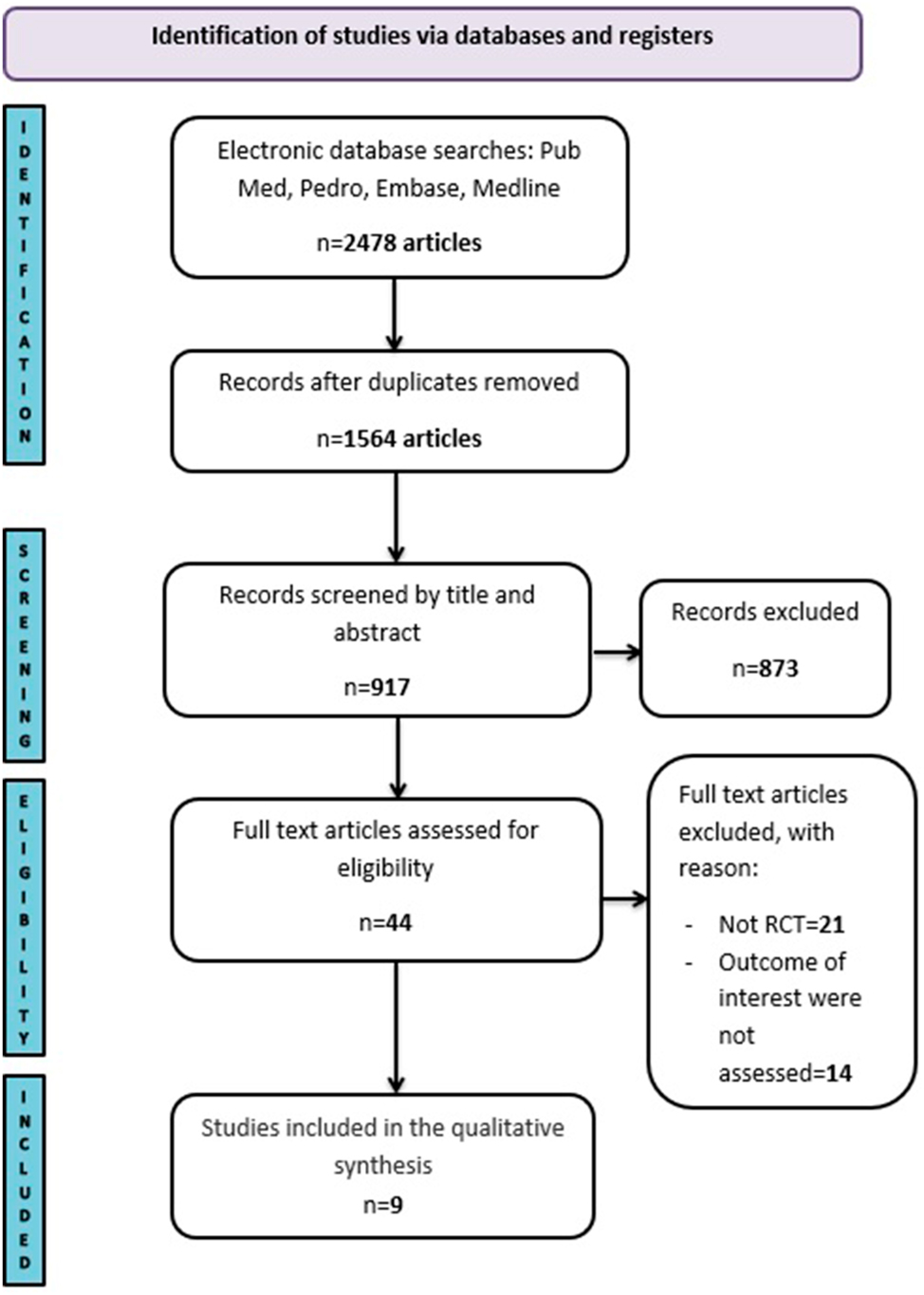
Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) 2020 flow diagram with the updated findings.
Filters were applied in various search engines to include eligible articles: studies involving human subjects, individuals over 65 years of age, and those receiving OMT. The included languages were English, Spanish, and Italian. It was not possible to assess racial or ethnic distinctions in the studies included in the review.
The excluded studies were literature reviews, study protocols, commentaries, personal contributions, unpublished works, and studies applying any form of manual medicine or technique not expressly osteopathic to the study group.
Information sources
To conduct a literature review on the effectiveness of OMT in the elderly population, four major medical databases were explored: PubMed (https://pubmed.ncbi.nlm.nih.gov/), Embase (https://www.embase.com), Google Scholar (http://scholar.google.it), SCOPUS (http://www.elsevier.com/onlinetools/scopus), ClinicalTrials.gov, Osteopathic Research Web (http://www.osteopathic-research.com/), and the Cochrane Library (http://www.thecochranelibrary.com) [22].
Search strategy
A combination of Medical Subject Headings (MeSH) terms and free-text terms with the Boolean operator “AND” were utilized: OMT, osteopathic manipulative treatment, osteopathic medicine, aging, older adult, elderly, aged, and geriatric people [23], 24].
Data items
The objective of this work is to review the effectiveness of OMT in addressing the pathologies of the elderly population. To date, the literature contains systematic reviews that analyze the effects of OMT on various conditions in older adults, but these references are limited to specific manual techniques. As a secondary objective, we aim to associate the outcome measures utilized in different studies with the various domains of intrinsic capacities outlined in the existing scientific literature concerning OMT and the elderly.
Results
A comprehensive bibliographic search identified a total of 2,478 articles. After removing 1,564 duplicates, 917 articles remained for screening. These were assessed based on their titles and abstracts, leading to the exclusion of 873 articles according to the established exclusion criteria.
In the final phase, the remaining 44 articles underwent a full-text evaluation. This process resulted in the exclusion of 21 articles that were not RCTs and 14 articles that did not meet the required outcome measures. Ultimately, a total of nine articles [25], [26], [27], [28], [29], [30], [31], [32], [33] were included in the systematic review (Table 1).
Study, study type, and aim of the study.
| Study | Study type | Aim of the study |
|---|---|---|
| Arienti et al. [25] | Nonrandomized controlled trial | Investigate the effect of OMT on reducing pain and improving quality of life in hospitalized geriatric cancer patients. |
| DiFrancisco-Donoghue et al. [26] | Randomized controlled trial | Determine whether OMT can improve motor function and balance in individuals with Parkinson’s disease. |
| Papa et al. [27] | Randomized controlled trial | Evaluate the effectiveness of OMT in patients with BPPV. |
| Noll et al. [28] | Randomized controlled trial | Asses the benefit of OMT in elderly patients with pneumonia. |
| Noll [29] | Randomized controlled trial | Verify the effectiveness of an osteopathic manipulative treatment protocol in improving lymphocyte count and lymphocyte subsets compared to a sham control group. |
| Snider et al. [30] | Randomized controlled trial | Investigating the benefits that elderly residents in a nursing home can receive from OMT. |
| Wieting et al. [31] | Randomized controlled trial | Measure the effects of OMT on the recovery of patients after CABG surgery |
| Zarucchi et al. [32] | Randomized controlled trial | Measure the effectiveness of OMT in Parkinsonian patients with Pisa syndrome |
| Papa et al. [33] | Randomized controlled trial | Assess the effectiveness of OMT on self-reported pain in elderly subjects with osteoporosis. |
-
BPPV, benign paroxysmal positional vertigo; CABG, coronary artery bypass grafting; OMT, osteopathic manipulative treatment.
The articles included in the review were published between 2012 and 2020, with five studies conducted in the USA [26], [28], [29], [30], [31] and four studies conducted in Italy [25], 27], 32], 33]. Among these, eight articles utilized a single-blind design [25], [26], [27], [28], [29], [30, 32], 33], and one article employed a double-blind design with numerical identifiers (31).
Of the included articles, eight were RCTs [26], [27], [28], [29], [30], [31], [32], [33], with only one article not being randomized [25]. All selected articles included participants aged 65 years and older, except for one study [31], which comprised two subgroups: the first included patients aged 50–74 years, and the second included patients aged 75 years and older (Table 2).
Characteristics of the studies included in the review.
| Study | Country of study | Measurement equipment | Single-blind or double-blind | Mean age, years | Sample size/sex | Statistical analysis tools | Dose, frequency, and duration of intervention | Major conclusion |
|---|---|---|---|---|---|---|---|---|
| Arienti et al. [25] | Italy | NRS | Single-blind | 76.50 ± 8.34 | 23 (14 women and 9 men) | Fisher’s exact test and Mann-Whitney U test | OMT: 1 time per week for 4 weeks, each session 45 min. Physiotherapy: 1 time per week for 4 weeks, each session 30 min. | Statistically significant pain relief; quality-of-life improvement not statistically significant. |
| DiFrancisco-Donoghue et al. [26] | USA | Mini-BESTest and MDS-UPDR. | Single-blind | 75 ± 16 | 9 (4 women and 5 men) | ANOVA | Bi-weekly treatments for 6 weeks. | No significant changes in balance (Mini-BESTest), but improved motor function (MDS-UPDR). |
| Papa et al. [27] | Italy | DHI and stabilometric platform | Single-blind | 57.5, 33–80 | 31 (10 women and 21 men) | SPSS version 22.0 | Treated group: 3 treatments over 3 weeks, each lasting 20 min. sham group: 3 treatments, each lasting 20 min (10 min of evaluation and 10 min of treatment). |
Significant improvement in DHI scores and reduced oscillation area on stabilometric platform. |
| Noll et al. [28] | USA | LOS, respiratory failure rate | Single-blind | Group 1: ages 50–74 years group 2: ages over 75 years |
387 patients | ITT analysis, PP analysis | OMT and LT treatments 2 times per day for the duration of the hospital stay. Each session lasted 20 min. | Statistically significant reduction in LOS for patients aged 50 to 74 in OMT group; decreased hospitalization rates for patients aged 75+. |
| Noll [29] | USA | Lymphocyte and white blood cell count via blood analysis | Single-blind | 65+ | 20 (17 women and 3 men) | ANOVA | One treatment lasting 6 min | Significant decrease in platelet count in OMT group; lymphocyte count and other parameters not statistically significant. |
| Snider et al. [30] | USA | Minimum data set | Single-blind | Age range (years): 74–96 | 21 (18 women and 3 men) | Kruskal-Wallis tests, ANCOVA | OMT group: received two treatments per month for 5 months (total of 10 treatments), with each intervention lasting 10–15 min. LT group: received two treatments per month for 5 months (total of 10 treatments), with each intervention lasting 5–10 min. |
Reduced hospitalizations and medication usage in OMT and LT groups compared to Tau group. |
| Wieting et al. [31] | USA | FIM | Double-blind with numeric identifiers | OMT: 65.1 placebo group: 67 control group: 63.3 |
53 (40 men and 13 women) | F tests, chi-square test | OMT group received one daily treatment in addition to standard care. | Significant improvements in functional recovery, hospital LOS, and time to postoperative bowel movement in OMT group. |
| Zarucchi et al. [32] | Italy | Diers formetric 4D | Single-blind | 67.7 | 24 (14 men and 10 women) | Chi-square test, t-tests, ANOVA | OMT group: 4 treatments in 30 days | Significant improvements in postural control and TLF in OMT group compared to sham group. |
| Papa et al. [33] | Italy | QUALEFFO-41 questionnaire and VAS | Single-blind | 77.2 | 72 (21 men and 51 women) | ANOVA and chi-square test | OMT group and placebo group. 6 weeks of intervention, 1 treatment per week. Duration 30 min. | No effect on pain (VAS); significant improvement in QUALEFFO-41 subscale. |
-
ANCOVA, analysis of covariance; ANOVA, analysis of variance; DHI, dizziness handicap inventory; FIM, functional independence measure; ITT, intention to treat; LOS, length of stay; LT, light touch; MDS-UPDRS, movement disorder society-sponsored revision of the unified Parkinson’s disease rating scale; Mini-BESTest, mini balance evaluation systems test; NRS, numeric rating scale; OMT, osteopathic manipulative treatment; PP, per protocol; SPSS, statistical package for the social sciences; TLF, trunk lateral flexion; VAS, visual analog scale.
Categorization of selected articles
We categorized the selected studies exploring the efficacy of OMT in geriatric populations into key thematic areas. These themes included Pain and Quality of Life, Balance, Hematological Parameters, Respiratory Conditions, and Postoperative Recovery.
Pain and quality of life
Three studies investigated the efficacy of OMT in alleviating pain among patients [25], 33], while one study focused on the enhancement of quality of life following OMT [30]. In the study [25], a total of 23 participants (14 women and nine men) were enrolled in a non-RCT. The primary objective of this study was to assess the effects of osteopathic manipulation on pain reduction and quality-of-life improvement in hospitalized geriatric oncology patients. Participants were assigned to one of two groups: the OMT group or the physical therapy group. The OMT group received treatment once a week for 4 weeks, with each session lasting 45 min. Conversely, the physical therapy group received treatment once a week for 4 weeks, with each session lasting 30 min. The study found a statistically significant improvement in pain relief; however, the improvement in quality of life did not reach statistical significance among the hospitalized geriatric oncology patients receiving OMT. Notably, the Numeric Rating Scale (NRS) scores significantly decreased in the OMT group at both T2 (p=0.004) and T4 (p=0.002), while the physical therapy group exhibited significant differences in two quality-of-life variables. Although there was an observed improvement in quality of life with OMT, it was not statistically significant. In the RCT by Papa et al. [33] 72 participants (21 men and 51 women) were enrolled to assess the effectiveness of OMT on self-reported pain in elderly individuals with osteoporosis. Participants were randomly assigned to either an OMT group or a placebo group. The intervention spanned 6 weeks, with one 30-min treatment session provided per week. Results indicated that OMT led to a significant reduction in disability compared to standard manipulative treatment (SMT), as reflected by a notable interaction in overall disability scores (p=0.001) and certain QUALEFFO-41 subscales, including mental well-being (p=0.058), health perception (p=0.005), and pain (p=0.003). However, no significant differences were observed between treatments for pain measured by the Visual Analog Scale (VAS) or in QUALEFFO-41 subscales assessing daily activities, walking, household cleaning, and leisure activities (p>0.05). Importantly, no adverse effects were reported during the study. In the study by Snider et al. [30] 21 participants (18 women and three men) were included. This RCT aimed to investigate the benefits that elderly residents in a nursing home could derive from OMT. Participants were allocated into three groups: the OMT group, the Light Touch group, and the Tau group. They received two treatments per month for 5 months (a total of 10 treatments). The intervention duration was 10–15 min for the OMT group and 10 min for the Light Touch group. The OMT and Light Touch groups had fewer hospitalizations (p=0.04), and the medications that were reduced are antibiotics for pneumonia and pain medications (p=0.001) compared with the TAU group.
Balance
Three studies assessed the impact of OMT on balance in geriatric patients [26], 27], 32]. The first study conducted by DiFrancisco-Donoghue et al. [26] utilized the Mini Balance Evaluation Systems Test (Mini-BESTest) as a measurement tool involving nine participants (4 women and five men). The primary objective was to determine whether OMT could improve motor function and balance in individuals with Parkinson’s disease. Participants received biweekly treatments over a 6-week period. The study utilized repeated-measures analysis of variance (ANOVA) to evaluate the effects of osteopathic manipulative medicine (OMM) compared to a control group across three measures: the Sensory Organization Test (SOT), Mini-BESTest, and Unified Parkinson’s Disease Rating Scale (MDS-UPDRS). For the SOT, the treatment effect was medium (partial η2=0.13) but not statistically significant (p=0.39). The OMM group demonstrated greater improvement in the composite SOT score from pre-to posttreatment (4.8 ± 5.1) compared to the control group (1.8 ± 6.0). This trend was particularly evident in the group that received control treatment for the first 6 weeks followed by OMM for the next 6 weeks (OMM: 4.8 ± 5.4; control: −1.0 ± 7.0). In the Mini-BESTest, no significant trends were observed in scores from pre-to postintervention for either group (p=0.21). Both groups showed slight positive improvements (OMM: 2.1 ± 2.4; control: 2.7 ± 2.7), but the treatment effect was small (partial η2=0.07) and not statistically significant (p=0.50). Regarding the MDS-UPDRS, the improvement in scores was greater from pre-to post-OMM (−1.7 ± 12.3) than in the control group (3.2 ± 10.7). This trend was more pronounced in the group that received the control for the first 6 weeks and then OMM for the subsequent 6 weeks (OMM: −7.5 ± 7.5; control: 3.0 ± 14.1). The treatment effect was large (partial η2=0.56) and statistically significant (p=0.021). In the second study by Papa et al. [27] the efficacy of OMT was evaluated in patients diagnosed with benign paroxysmal positional vertigo (BPPV). The study included 31 participants (10 women and 21 men) and employed the Dizziness Handicap Inventory (DHI) along with a stabilometric platform for assessment. Participants were randomly assigned to one of two groups: the OMT group received three treatments over 3 weeks, each lasting 20 min, while the sham group (SG) received three treatments of 10 min each over the same timeframe. Results demonstrated a significant improvement in overall DHI scores and a reduction in the area of oscillation measured on the stabilometric platform, indicating enhanced balance. After the treatment, the treatment group (TG) demonstrated significant improvements in the DHI compared to the control group (SG). The global DHI score improved (p=0.02), along with functional and physical components (both p=0.03). Additionally, the swinging area decreased significantly (p=0.02), indicating enhanced stability. Strong positive associations were found between changes in the swinging area and lifestyle measures in the TG: global measures (r=0.53, p=0.02), functional measures (r=0.50, p=0.03), and physical measures (r=0.60, p=0.01). This indicates that better stability correlates with improvements in lifestyle factors. The final study by Zarucchi et al. [32] utilized the Diers Formetric C4D system to evaluate the effectiveness of OMT in individuals with Parkinson’s disease and Pisa syndrome. Participants were allocated to two groups: 12 in the OMT group (maximal increase in resting tension [MIRT] + OMT) and 12 in the sham OMT group (MIRT + sham OMT). Each group received one treatment per week for 30 days. The OMT group exhibited significant improvements in postural control and trunk lateral flexion (TLF) compared to the SG, suggesting the potential of OMT to enhance balance in this patient population. One month after treatment, the sway area in the OMT group showed a significant decrease compared to the placebo group, with a mean change (delta) of −326.00 ± 491.24 mm2 and a p value of 0.01, indicating an improvement in stability. Additionally, in the experimental group, trunk lateral flexion (TLF) demonstrated a mean inclination reduction of 3.33° after treatment, with a p value of 0.044 and a mean effect size (d) of 0.54, suggesting a positive impact of the treatment. A significant positive association was also observed between the change in sway area (delta ECSA) and the change in TLF (delta TLF), with a p value of 0.04 and a correlation coefficient (r) of 0.46, indicating that an improvement in stability is associated with an increase in trunk lateral flexibility.
Hematological parameters
One trial conducted by Noll et al. [29] examined the efficacy of OMT on lymphocyte count in comparison to a control group. The study recruited 20 participants (17 females and three males), who were randomly assigned to one of two groups: the OMT group and the control group. The OMT group underwent 6 min of treatment, which included three techniques: thoracic myofascial release, splenic pump, and lymphatic pump. In contrast, the control group received a light-touch treatment for 30 min, targeting the same anatomical areas as those treated in the OMT group. Hematological analyses were performed 30 min posttreatment. No statistically significant differences were observed in lymphocyte subsets between groups, even though the OMT group showed a mean reduction of −117 (SD 221) lymphocyte cells per microliter compared to an increase of 87 (SD 271) in the Light Touch group (p=0.08). The platelet counts differed significantly, with a mean decrease of 15,400 (SD 7947) per microliter in the OMT group vs. an increase of 4,700 (SD 17,857) in the Light Touch group (p=0.004). Although red blood cell count, hemoglobin, and hematocrit also decreased in the OMT group, these changes were not statistically significant.
Respiratory conditions
A study was conducted to evaluate the efficacy of OMT in elderly patients diagnosed with pneumonia, specifically analyzing the impact on length of stay (LOS) associated with respiratory failure, a cohort of 387 patients was examined [28]. Participants were randomly assigned to either the OMT group or the Light Touch control group, with both receiving treatment twice daily, each session lasting 20 min throughout their hospital stay. The findings revealed a statistically significant reduction in LOS for adults aged 50–74 years in the OMT group, although there was a notable decrease in hospitalization rates among participants aged 75 and older. In a per-protocol analysis of the younger age subgroup, the LOS was significantly shorter for the OMT group (median, 2.9 days; n=43) compared to the Light Touch group (median, 3.7 days; n=45) and conventional care only (CCO) (median, 4.0 days; n=65) groups (p=0.006). In an intention-to-treat analysis of the older-age subgroup, in-hospital mortality rates were lower for the OMT group (1 of 66 [2 %]) and Light Touch group (2 of 68 [3 %]) compared to the CCO group (9 of 67 [13 %]) (p=0.005). Furthermore, in the PSI class IV subgroup, the OMT group had a shorter LOS than the CCO group (median: 3.8 days [n=40] vs. 5.0 days [n=50]; p=0.01) and a lower rate of ventilator-dependent respiratory failure (0 of 40 [0 %] vs. 5 of 50 [10 %]; p=0.05). Additionally, the PSI class V subgroup’s intention-to-treat analysis showed lower in-hospital mortality rates for the OMT group (1 of 22 [5 %]) compared to the CCO group (6 of 19 [32 %]) (p=0.05), but no significant difference was observed compared to the Light Touch group (2 of 15 [13 %]).
Postoperative recovery following cardiovascular surgery
One study [31] involved 53 subjects (40 men and 13 women) to evaluate the effects of OMT on the recovery of patients following coronary artery bypass grafting (CABG). The participants were divided into three groups: 17 in the OMT group, 18 in the Placebo group, and 18 in the Control group. The OMT group received one daily treatment in addition to standard care, whereas the Placebo group received light-touch treatment alongside standard care. The Control group received only standard postoperative care. Primary outcome measures included length of hospital stay, time to postoperative bowel movement, and Functional Independence Measure (FIM) scores. The study found that the OMT protocol significantly improved functional recovery in patients undergoing CABG surgery compared to the other groups. The average discharge times after surgery were 6.1 (1.4) days for the OMT group, 6.3 (1.5) days for the placebo group, and 6.7 (3.0) days for the control group. Notably, patients in the OMT group were discharged 0.55 days earlier than those in the control group and 0.16 days earlier than those in the placebo group. Additionally, the mean time to the first postoperative bowel movement was shorter in the OMT group at 3.5 (0.9) days, compared to 4.0 (0.8) days for both the placebo and control groups. On day 3 after surgery, the total FIM scores indicated improved functional independence in the OMT group, with a mean score of 19.3 (6.7), compared to 15.4 (7.3) for the placebo group and 18.6 (6.5) for the control group. The OMT group’s score was 0.81 points higher than the control and 3.87 points higher than the placebo group. However, it is important to note that none of these differences reached statistical significance (p<0.05).
Discussion
This scoping review aimed to map the existing evidence regarding the efficacy of OMT for various health conditions affecting the elderly population. The analysis of selected studies reveals several key themes concerning the application of OMT and its potential benefits in geriatric care. The review highlights that OMT may offer significant relief in pain management for elderly patients, as evidenced by studies such as those conducted by Arienti et al. [25] and Papa [33]. These findings suggest that OMT can be an effective nonpharmacological intervention to alleviate pain in this demographic, particularly in populations with chronic conditions. However, although some studies reported improvements in quality of life, such as the work by Snider et al. [30] the results were not always statistically significant, indicating the need for more rigorous research designs. Furthermore, the impact of OMT on balance and functional independence emerged as a notable area of interest. Research by Papa [27] and Zarucchi et al. [32] indicates that OMT can contribute to better balance and mobility, which are essential factors in reducing fall risk among older adults.
All RCTs included in this review utilized OMT protocols for the administration of the intervention [25], [26], [27], [28], [29], [30], [31], [32], except for the 2012 study by Papa et al. [33] which employed a “treat what you find” methodology.
Behavioral interventions aimed at promoting physical activity for the management of cardiovascular disease, diabetes, osteoporosis, and other geriatric conditions should incorporate resistance training and structured exercise programs. Enhancing pain management and improving balance are critical factors that can significantly increase adherence to lifestyle modifications, thereby optimizing therapeutic outcomes.
Given that falls are a major cause of morbidity in this population, these findings underscore the importance of integrating OMT into broader fall prevention strategies. Despite the promising evidence, this review identified several limitations in the current literature. Variability in methodologies, sample sizes, and outcome measures across studies complicates the interpretation of findings and their generalizability. Additionally, there remains a scarcity of long-term follow-up studies, which are crucial for assessing the sustained impact of OMT on geriatric health outcomes.
This scoping review has some potential limitations that should be acknowledged. First, the methodological heterogeneity of the included studies may affect the generalizability of the findings. Second, the lack of longitudinal data limits the ability to draw robust conclusions on the long-term effects of OMT interventions. Finally, potential selection biases may arise from the inclusion of studies available only in specific languages or geographic contexts, which could influence the comprehensiveness of the review. In conclusion, while this scoping review provides insights into the potential benefits of OMT for the elderly population, it also highlights the need for further research to address existing gaps. Future studies should focus on developing standardized protocols, defining comprehensive outcome measures, and exploring the long-term effects of OMT within integrated geriatric care models. By doing so, the scientific community can better understand the role of OMT in enhancing the health and well-being of older adults.
Conclusions
The review highlights the crucial role of OMT in improving pain, balance, and quality of life in geriatric patients. These findings demonstrate that OMT is a valuable therapeutic approach that enhances personalized healthcare for this population. Incorporating OMT into osteopathic practice may lead to significant benefits in the well-being of elderly patients, promoting healthier aging. Moreover, this study encourages further research into the full potential of OMT. In summary, our findings advocate for integrating OMT as a key element of osteopathic care for geriatric patients.
-
Research ethics: The research was conducted in accordance with the ethical principles established by the Declaration of Helsinki.
-
Informed consent: Not applicable.
-
Author contributions: All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
-
Use of Large Language Models, AI and Machine Learning Tools: None declared.
-
Conflict of interest: None declared.
-
Research funding: None declared.
-
Data availability: Not applicable.
References
1. World Health Organization (WHO). World report on aging and health. Geneva: WHO Press; 2021.Search in Google Scholar
2. United Nations. World population ageing 2019: highlights. New York: United Nations; 2019.Search in Google Scholar
3. Hunter, DJ, Bierma-Zeinstra, S. Osteoarthritis. Lancet 2019;393:1745–59. https://doi.org/10.1016/s0140-6736(19)30417-9.Search in Google Scholar PubMed
4. Clynes, MA, Gregson, CL, Bruyère, O. Osteoporosis and fracture risk in older people. Osteoporos Int 2020;31:3–16.Search in Google Scholar
5. Zhou, Z. The impact of diabetes on healthcare costs and quality of life. J Diabet Complicat 2021;35:107–12.Search in Google Scholar
6. Benjamin, EJ, Muntner, P, Alonso, A, Bittencourt, MS, Callaway, CW, Carson, AP, et al.. Heart disease and stroke statistics—2019 update: a report from the American Heart Association. Circulation 2019;139:e56–528. https://doi.org/10.1161/cir.0000000000000659.Search in Google Scholar
7. GBD Chronic Respiratory Disease Collaborators. Global burden of chronic respiratory diseases and risk factors, 1990–2017: a systematic analysis. Lancet Respir Med 2020;8:585–96. https://doi.org/10.1016/S2213-2600(20)30105-3.Search in Google Scholar PubMed PubMed Central
8. McPartland, JM, Sullivan, SJ. Osteopathic manipulative treatment and the elderly: a systematic review. Am J Osteopath Med 2015;115:375–84.Search in Google Scholar
9. Di Stefano, A, D’Angelo, M. The role of osteopathic treatment in the management of chronic pain: a systematic review. Int J Osteopath Med 2018;27:14–23.10.1016/j.ijosm.2017.10.005Search in Google Scholar
10. Licciardone, JC, Gatchel, RJ, Phillips, N. The impact of osteopathic manipulative treatment on chronic low back pain: a systematic review. J Am Osteopath Assoc 2013;113:691–700.Search in Google Scholar
11. Cummings, TM, White, AR. Evidence-based clinical guidelines for osteopathic manipulative treatment for the management of chronic low back pain. J Bodyw Mov Ther 2015;19:678–87.Search in Google Scholar
12. Gatterman, MI. Osteopathic manipulative treatment for chronic pain in the elderly: a review. Clin Geriatr 2005;13:125–30.Search in Google Scholar
13. Stuber, K, Baker, J, Adams, J. Osteopathic manipulative treatment in the management of patients with knee osteoarthritis: a randomized controlled trial. J Pain 2017;18:482–9.Search in Google Scholar
14. Fronczek, R, Demaerschalk, BM, Hentz, JG. The effectiveness of osteopathic manipulation on the clinical features of Pisa syndrome in elderly patients with Parkinson’s disease: a case series. J Parkinsons Dis 2020;10:89–97.Search in Google Scholar
15. Bäuerle, A, Bäuerle, T. Effects of exercise on fall prevention and physical performance in older adults: a systematic review. Arch Gerontol Geriatr 2017;68:29–36.Search in Google Scholar
16. Chaves, GS, Nedel, FB, de Carvalho, T. Effect of physiotherapy intervention on balance and quality of life in elderly individuals: a systematic review. Physiother Theory Pract 2018;34:69–79.Search in Google Scholar
17. Goerl, K, Carter, T, Bacharach, H. The effectiveness of chiropractic manipulation in the treatment of chronic pain: a systematic review. J Chiropr Med 2016;15:29–38.Search in Google Scholar
18. Coulter, ID, Herman, PM, Kominski, GF. Chiropractic care for low back pain: a systematic review. J Manip Physiol Ther 2016;39:59–72.Search in Google Scholar
19. Chikly, B, Sills, M. The effectiveness of craniosacral therapy for patients with fibromyalgia: a systematic review. J Bodyw Mov Ther 2014;18:72–7.Search in Google Scholar
20. Vickers, AJ, Vertosick, EA, Lewith, G, MacPherson, H, Foster, NE, Sherman, KJ, et al.. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain 2018;19:222–9.10.1016/j.jpain.2017.11.005Search in Google Scholar PubMed PubMed Central
21. Tricco, AC, Lillie, E, Zarin, W, O’Brien, KK, Colquhoun, H, Levac, D, et al.. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. https://doi.org/10.7326/m18-0850.Search in Google Scholar
22. Bramer, WM, Rethlefsen, ML, de Jonge, GB, Mast, F, Kleijnen, J. A systematic approach to searching: an efficient and complete method to develop literature searches. J Med Libr Assoc 2017;105:421–31.Search in Google Scholar
23. Booth, A, Sutton, A, Papaioannou, D. Searching for qualitative research for inclusion in systematic reviews: a structured methodological review. Syst Rev 2021;10:60.Search in Google Scholar
24. Lefebvre, C, Glanville, J, Wieland, LS, Coles, B, Weightman, AL. Methodological developments in searching for systematic reviews: past, present and future. Cochrane Database Syst Rev 2020;2020.Search in Google Scholar
25. Arienti, C, Bosisio, T, Ratti, S, Miglioli, R, Negrini, S. Osteopathic manipulative treatment effect on pain relief and quality of life in oncology geriatric patients: a nonrandomized controlled clinical trial. Integr Cancer Ther 2018;17:1163–71. https://doi.org/10.1177/1534735418796954.Search in Google Scholar PubMed PubMed Central
26. DiFrancisco-Donoghue, J, Apoznanski, T, de Vries, K, Jung, MK, Mancini, J, Yao, S. Osteopathic manipulation as a complementary approach to Parkinson’s disease: a controlled pilot study. NeuroRehabilitation 2017;40:145–51. https://doi.org/10.3233/NRE-161400.Search in Google Scholar PubMed
27. Papa, L, Amodio, A, Biffi, F, Mandara, A. Impact of osteopathic therapy on proprioceptive balance and quality of life in patients with dizziness. J Bodyw Mov Ther 2017;21:866–72. https://doi.org/10.1016/j.jbmt.2017.03.001.Search in Google Scholar PubMed
28. Noll, DR, Degenhardt, BF, Johnson, JC. Multicenter osteopathic pneumonia study in the elderly: subgroup analysis on hospital length of stay, ventilator-dependent respiratory failure rate, and in-hospital mortality rate. J Am Osteopath Assoc 2016;116:574–87. https://doi.org/10.7556/jaoa.2016.117.Search in Google Scholar PubMed
29. Noll, DR. The short-term effect of a lymphatic pump protocol on blood cell counts in nursing home residents with limited mobility: a pilot study. J Am Osteopath Assoc 2013;113:520–8. https://doi.org/10.7556/jaoa.2013.003.Search in Google Scholar PubMed
30. Snider, KT, Snider, EJ, Johnson, JC, Hagan, C, Schoenwald, C. Preventative osteopathic manipulative treatment and the elderly nursing home resident: a pilot study. J Am Osteopath Assoc 2012;112:489–501.Search in Google Scholar
31. Wieting, JM, Beal, C, Roth, GL, Gorbis, S, Dillard, L, Gilliland, D, et al.. The effect of osteopathic manipulative treatment on postoperative medical and functional recovery of coronary artery bypass graft patients. J Am Osteopath Assoc 2013;113:384–93.Search in Google Scholar
32. Zarucchi, A, Vismara, L, Frazzitta, G, Mauro, A, Priano, L, Maestri, R, et al.. Efficacy of osteopathic manipulative treatment on postural control in Parkinsonian patients with Pisa syndrome: a pilot randomized placebo-controlled trial. NeuroRehabilitation 2020;46:529–37. https://doi.org/10.3233/NRE-203068.Search in Google Scholar PubMed
33. Papa, L, Mandara, A, Bottali, M, Gulisano, V, Orfei, S. A randomized control trial on the effectiveness of osteopathic manipulative treatment in reducing pain and improving the quality of life in elderly patients affected by osteoporosis. Clin Cases Miner Bone Metab 2012;9:179–83.Search in Google Scholar
© 2025 the author(s), published by De Gruyter, Berlin/Boston
This work is licensed under the Creative Commons Attribution 4.0 International License.

