Abstract
Objectives
To establish a practical and valid method for the diagnosis of twin gestation in uteri with Müllerian anomalies in the first trimester of pregnancy.
Case presentation
This was a prospective cohort study. Two cases with congenital uterine anomalies were followed prospectively from 7 weeks of gestation and compared to eight controls. The longitudinal to transverse uterine lumen diameter ratio (LTDR) was measured in mid-sagittal and coronal planes. The LTDR was compared between unicornuate and didelphys uteri to normal uteri controls weekly. The area under the curve for the coronal and sagittal planes were 1.000 and 0.823, respectively. For the coronal plane, an LTDR of 1.15 was selected as optimal for predicting uteri with a Müllerian anomaly, with a sensitivity of 100%, specificity of 100%. An LTDR of 1.68 in the sagittal plane was selected as optimal for predicting anomalous uteri, with a sensitivity of 100%, specificity of 73%.
Conclusions
LTDR ratios measured in mid sagittal and coronal planes of unicornuate and didelphys uteri with twin gestation during the first trimester of pregnancy are highly predictive of Müllerian anomalies. Early diagnosis of uterine anomalies could provide a reference to initiate earlier meticulous follow-up.
Introduction
During the reproductive life, congenital anomalies can cause clinical symptoms and obstetrical complications. Only a minority of uterine anomalies are diagnosed following clinical signs such as pelvic pain, primary amenorrhea, dysmenorrheal and dyspareunia. The majority of them are diagnosed following an obstetrical complication such as recurrent pregnancy losses, premature labor, fetal mal-presentations and fetal demise [1].
Müllerian anomalies are classified into six classes according to the American Fertility Society [2] classification. Didelphys and unicornuate uteri are the result of unification defects of the two Müllerian ducts. In common, these two anomalies are formed with one or two functioning uterine horns. The rate of Müllerian anomalies in an unselected population is between 4.3% and 6.7% [3], [4], [5], [6], [7]. Unicornuate uterus prevalence is higher in infertile patients [8]. Obstetrical complications are more common in unicornuate uteri than didelphic uteri [9]. The anatomic and functional defects of a unicornuate uterus may lead to a poor tolerance especially in twin pregnancies and result in more serious adverse obstetrical outcomes.
The occurrence of multifetal gestations in a unicornuate or didelphys uteri carries a high risk for obstetrical complications such as increased incidence of early and late miscarriage, preterm delivery and fetal growth retardation and fetal demise [10]. Early diagnosis of these uterine anomalies during the first trimester of pregnancy is paramount to early initiation of meticulous obstetric management. Hitherto, there are no reports of a valid method to diagnose Müllerian anomalies during twin pregnancy. Therefore, we aim to establish a practical method for the diagnosis of unicornuate and didelphic uteri with twin gestation during the first trimester of pregnancy.
Case presentation
Ten patients with twin gestations were included in the study, eight with normal uteri, one with a unicornuate uterus and one with a didelphys uterus, both with a pre-conception diagnosis of a Müllerian anomaly by three-dimensional (3D) ultrasound. They underwent 3D ultrasound scans weekly, from 7 to 12 weeks’ gestation, (GE Voluson 730 expert, abdominal and vaginal probe) (General Electric, Zipf, Austria). Measurements of the ratio between the longitudinal and the transverse uterine lumen diameter (LTDR) in the sagittal and coronal planes were applied to all patients. Transvaginal and abdominal 3D ultrasound (U/S) scans were performed using a multi-planar method weekly from 7 to 12 weeks. Immediately after applying trans-vaginal 3D volume acquisition of the uterus, the sagittal and coronal planes were displayed on a screen concomitantly. The sagittal plane was manipulated until the fundal uterine lumen was displayed concomitantly with the internal cervical os, and then a longitudinal measurement of uterine lumen was performed. The longitudinal diameter was measured between the center of the fundal lumen and the internal os. The transverse diameter was measured perpendicular to the longitudinal diameter, bisecting the longitudinal diameter and in between the right and left internal uterine walls. The same definition of measurements was applied in the sagittal and coronal planes (Figure 1). The mean LTDR for the sagittal and coronal planes were compared and analyzed between Müllerian uteri and normal uteri (Figure 2 and Figure 3).

Normal uterus with 7-week twin gestation.
Left: sagittal plane of uterus. Right: volume contrast imaging ultrasound of the coronal plane demonstrating double sacs of twin gestation.

Unicornuate uterus with 10-week twin pregnancy.
Left: sagittal plane of uterus showing the line of the coronal plane that is displayed on the right-side image. Right: VCI-C showing the narrow shape structure of the unicornuate uterus.

Uterus didelphys with 10-week twin gestation in the same horn of the uterus.
Left: sagittal plane of the uterus. Right: volume contrast imaging of the coronal plane. Measurements cursors demonstrate the following: 1 = longitudinal length, 2 = anterior-posterior length, 3 = longitudinal length, 4 = transverse length.
The study was approved by the hospital Ethics Committee.
Results
A total of 120 measurements of LTDR were performed weekly from 7 to 12 weeks gestation in ten pregnant women with twin gestation in the coronal and midsagittal planes. Eight of these patients had normal uteri, one had a unicornuate uterus and one had a didelphys uterus. Mean and standard deviation of LTDRs in the coronal plane during first trimester of pregnancy and in the mid-sagittal plane are shown in Table 1 and Table 2. Mean sagittal and coronal LTDRs of the uteri with Müllerian anomalies [2.08 ± 0.26 (range 1.7–2.36) and 2.1 ± 0.21 (range 1.7–2.4), respectively] were significantly higher (P < 0.01) compared to normal uteri [1.61 ± 0.43 (range 1.05–2.6) and 0.92 ± 0.12 (range 0.72–1.15), respectively].
3D U/S measurements of the ratio between the longitudinal and the transverse uterine lumen diameter (LTDR) in the sagittal plane.
| Weeks in pregnancy | 7 | 8 | 9 | 10 | 11 | 12 |
| Müllerian anomaly | 2.3 | 1.9 | 1.94 | 2.11 | 2.12 | 1.72 |
| Normal uterus | 1.48 | 0.98 | 1.47 | 1.76 | 1.8 | 1.3 |
3D U/S measurements of the ratio between the longitudinal and the transverse uterine lumen diameter (LTDR) in the coronal plane.
| Weeks in pregnancy | 7 | 8 | 9 | 10 | 11 | 12 |
| Müllerian anomaly | 2.3 | 1.9 | 1.94 | 2.11 | 2.12 | 1.72 |
| Normal uterus | 0.9 | 0.98 | 0.95 | 0.87 | 0.94 | 0.86 |
A schematic illustration of a normal and unicornuate uterus enlargement is presented in Figure 4. We used a receiver operator characteristic curve to determine the optimal sensitivity and specificity for the detection of an anomalous uterus (Figure 5). The area under the curve for the coronal and sagittal planes were 1.000 and 0.823, respectively. For the coronal plane, an LTDR of 1.15 was selected as optimal for predicting uteri with a Müllerian anomaly, with a sensitivity of 100%, specificity of 100%. An LTDR of 1.68 in the sagittal plane was selected as optimal for predicting anomalous uteri, with a sensitivity of 100%, specificity of 73% (Figure 5).
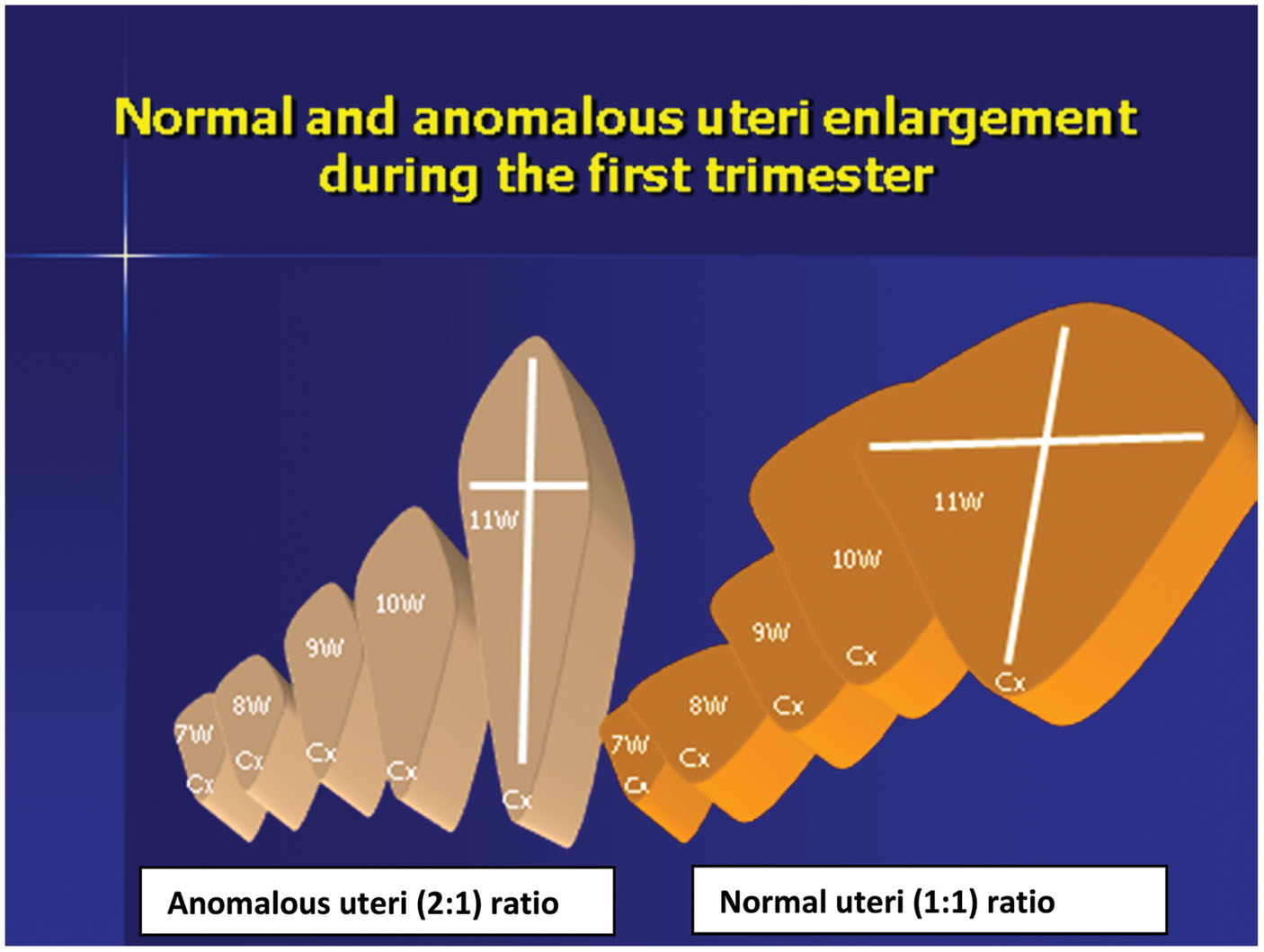
A schematic illustration of a normal and anomalous uteri enlargement during the first trimester from week 7 to 11 of gestation.

Receiver operating characteristic (ROC) curve analysis of longitudinal to transverse uterine lumen diameter ratio in the coronal plane.
(A) Area under the ROC curve 1.000. Cut-off point < 1.15 sensitivity 100% specificity 100%, (CI 69–100) PPV 100%. ROC curve analysis of longitudinal to transverse uterine lumen diameter ratio in the sagittal plane. (B) Area under the ROC curve 0.823. Cut-off point < 1.68 sensitivity 100% specificity 73%.
Discussion
The results of this case series showed that the LTDR is a novel method for the diagnosis of twin pregnancy in unicornuate and didelphic uteri during the first trimester.
The implantation of twin gestational sacs in one lumen of these two Müllerian anomalies is very rare. Relatively more common is the implantation of twin pregnancy in two separate lumens of didelphys uterus. The increased risk for complications in pregnancy due to Müllerian anomalies makes early diagnosis imperative, especially in the case of twin pregnancies [6], [8], [10], [11].
A unicornuate uterus is a Müllerian anomaly with prognostic implications for poor outcomes during pregnancy. The risk for adverse obstetric outcome increases with a twin pregnancy. The incidence of twin pregnancy in the same horn of a uterus didelphys is extremely rare with a single case reported [11]. Although a normal course of pregnancy is possible in both anomalies discussed above, the risk for complications is considerably high, and early diagnosis of twin pregnancies in anomalous uteri is of paramount significance.
It is unclear whether interventions before conception or early in pregnancy such as resection of the rudimentary horn, prophylactic cervical cerclage or progesterone therapy decidedly improve obstetrical outcomes. Current practice suggests that such interventions may be helpful [12], [13], [14], [15].
Diagnosis of Müllerian anomalies by transvaginal 3D ultrasounds is more cost-effective and less invasive than hysterosalpingography and magnetic resonance imaging and allows patients to avoid the risks of receiving radiation and/or iodinated contrast [16], [17], [18].
When a patient presents late in the first-trimester with a twin pregnancy, the sonographer might experience technical difficulties in demonstrating a rudimentary horn in a case of unicornuate uterus or a second uterine cavity in a case of uterus didelphys.
If the sonographer suspects an abnormal uterine contour or size in a patient with no past medical history of uterine anomaly and a twin pregnancy presenting in the first-trimester, the LTDR measurement is a simple technique with high sensitivity for diagnosing an anomalous gravid uterus.
Women presenting with a history of the aforementioned anomalies should be considered high-risk for obstetrical complications.
This study is the first to use 3D technology for the measurements of uterine longitudinal and transverse diameters. We demonstrate a simple technique that can be used by 3D ultrasound users to differentiate between unicornuate and didelphys uterus from a normal uterus. The measurement can be obtained in the mid sagittal or coronal plane with equal diagnostic accuracy.
In conclusion, the LTDR is a novel mean to achieve early detection of a gravid uterus with Müllerian anomalies and perhaps by that, reduce miscarriages and improve obstetric outcomes.
-
Ethical approval: The research related to human use has complied with all the relevant national regulations, institutional policies and has been conducted in accordance with the tenets of the Helsinki Declaration, and it has been approved by the authors’ Institutional Review Board or equivalent committee.
-
Author contributions: All the authors have accepted responsibility for the entire content of this manuscript and approved the submission. Efraim Zohav and Leonti Grin have equally contributed equally to this study
-
Research funding: None declared.
-
Employment or leadership: None declared.
-
Honorarium: None declared.
-
Competing interests: The funding organization(s) played no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the report for publication.
References
[1] Bermejo C, Martínez-Ten P, Recio M, Ruiz-López L, Díaz D, Illescas T. Three-dimensional ultrasound and magnetic resonance imaging assessment of cervix and vagina in women with uterine malformations. Ultrasound Obstet Gynecol. 2014;43:336–45.10.1002/uog.12536Search in Google Scholar
[2] Markov D, Slavchev B, Markov P, Apostolova M. [Asymmetric obstructed uterus didelphys/incomplete Herlyn-Werner-Wunderlich syndrome/diagnosed by transvaginal 3D ultrasound–a case report]. Akush Ginekol (Sofiia). 2009;48:47–51.Search in Google Scholar
[3] Caliskan E, Ozkan S, Cakiroglu Y, Sarisoy HT, Corakci A, Ozeren S. Diagnostic accuracy of real-time 3D sonography in the diagnosis of congenital Mullerian anomalies in high-risk patients with respect to the phase of the menstrual cycle. J Clin Ultrasound. 2010;38:123–7.10.1002/jcu.20662Search in Google Scholar
[4] Al Kaissi A, Ganger R, Hofstaetter JG, Klaushofer K, Grill F. The aetiology behind torticollis and variable spine defects in patients with Müllerian duct/renal aplasia-cervicothoracic somite dysplasia syndrome: 3D CT scan analysis. Eur Spine J. 2011;20:1720–7.10.1007/s00586-011-1835-1Search in Google Scholar
[5] Simón C, Martinez L, Pardo F, Tortajada M, Pellicer A. Müllerian defects in women with normal reproductive outcome. Fertil Steril. 1991;56:1192–3.10.1016/S0015-0282(16)54741-4Search in Google Scholar
[6] Chan YY, Jayaprakasan K, Zamora J, Thornton JG, Raine-Fenning N, Coomarasamy A. The prevalence of congenital uterine anomalies in unselected and high-risk populations: a systematic review. Hum Reprod Update. 2011;17:761–71.10.1093/humupd/dmr028Search in Google Scholar
[7] Grimbizis GF, Di Spiezio Sardo A, Saravelos SH, Gordts S, Exacoustos C, Van Schoubroeck D, et al. The Thessaloniki ESHRE/ESGE consensus on diagnosis of female genital anomalies. Gynecol Surg. 2016;13:1–16.10.1007/s10397-015-0909-1Search in Google Scholar
[8] Reichman D, Laufer MR, Robinson BK. Pregnancy outcomes in unicornuate uteri: a review. Fertil Steril. 2009;91:1886–94.10.1016/j.fertnstert.2008.02.163Search in Google Scholar
[9] Moutos DM, Damewood MD, Schlaff WD, Rock JA. A comparison of the reproductive outcome between women with a unicornuate uterus and women with a didelphic uterus. Fertil Steril. 1992;58:88–93.10.1016/S0015-0282(16)55141-3Search in Google Scholar
[10] Li X, Ouyang Y, Yi Y, Lin G, Lu G, Gong F. Pregnancy outcomes of women with a congenital unicornuate uterus after IVF-embryo transfer. Reprod Biomed Online. 2017;35:583–91.10.1016/j.rbmo.2017.07.015Search in Google Scholar
[11] Kanakas N, Boos R, Schmidt W. Twin pregnancy in the right horn of a uterus didelphys: a case report. Eur J Obstet Gynecol Reprod Biol. 1989;32:287–92.10.1016/0028-2243(89)90049-XSearch in Google Scholar
[12] Ng KS, Ng BK, Lim PS, Shafiee MN, Abdul Karim AK, Omar MH. Use of hydroxyprogesterone caproate to prevent preterm labour in uterine didelphys: a case report. Horm Mol Biol Clin Investig. 2016;27:89–91.10.1515/hmbci-2015-0060Search in Google Scholar PubMed
[13] Abramovici H, Faktor JH, Pascal B. Congenital uterine malformations as indication for cervical suture (cerclage) in habitual abortion and premature delivery. Int J Fertil. 1983;28:161–4.Search in Google Scholar
[14] Golan A, Langer R, Wexler S, Segev E, Niv D, David MP. Cervical cerclage--its role in the pregnant anomalous uterus. Int J Fertil. 1990;35:164–70.10.1097/00006254-199103000-00009Search in Google Scholar
[15] Leo L, Arduino S, Febo G, Tessarolo M, Lauricella A, Wierdis T, et al. Cervical cerclage for malformed uterus. Clin Exp Obstet Gynecol. 1997;24:104–6.Search in Google Scholar
[16] Armstrong L, Fleischer A, Andreotti R. Three-dimensional volumetric sonography in gynecology: an overview of clinical applications. Radiol Clin North Am. 2013;51:1035–47.10.1016/j.rcl.2013.07.005Search in Google Scholar PubMed
[17] Faivre E, Fernandez H, Deffieux X, Gervaise A, Frydman R, Levaillant JM. Accuracy of three-dimensional ultrasonography in differential diagnosis of septate and bicornuate uterus compared with office hysteroscopy and pelvic magnetic resonance imaging. J Minim Invasive Gynecol. 2012;19:101–6.10.1016/j.jmig.2011.08.724Search in Google Scholar PubMed
[18] Robbins JB, Parry JP, Guite KM, Hanson ME, Chow LC, Kliewer MA, et al. MRI of pregnancy-related issues: müllerian duct anomalies. AJR Am J Roentgenol. 2012;198:302–10.10.2214/AJR.11.7789Search in Google Scholar PubMed
©2019 Walter de Gruyter GmbH, Berlin/Boston
Articles in the same Issue
- Case Reports – Obstetrics
- Extended multi-drug maternal therapy for refractory supraventricular tachycardia in premature hydrops fetalis
- Rare etiology of arthrogryposis multiplex congenita at term: congenital cytomegalovirus infection
- Mosaic trisomy 15 and prenatal genetic counselling: a case of Prader-Willi syndrome due to maternal uniparental disomy
- Prenatal detection and obstetric management of true umbilical cord knots using color Doppler and 4D ultrasonography: a report of two cases and literature review
- Three laparotomies later: extrinsic duodenal atresia from malrotation complicated by intrinsic duodenal and pyloric windsock webs
- Prenatal diagnosis of 17-hydroxylase/17,20-lyase deficiency (17OHD) in a case of 46,XY sex discordance and low maternal serum estriol
- Case Reports – Fetus
- A transient finding of fetal head entrapment caught in a uterine synechium or amniotic band
- Uncovering new physiology in bilateral renal agenesis following amnioinfusion
- Prenatal diagnosis of congenital mirror foot: case report and review
- A full-term infant with type II thanatophoric dysplasia
- Twin pregnancy in uteri with congenital anomalies: prenatal diagnosis by three- dimensional ultrasound
- Case Reports – Newborn
- Neonatal hemorrhagic shock as a consequence of ruptured velamentous vessels – a report of two cases
- Congenital multinodular goiter in a neonate presenting with airway obstruction
Articles in the same Issue
- Case Reports – Obstetrics
- Extended multi-drug maternal therapy for refractory supraventricular tachycardia in premature hydrops fetalis
- Rare etiology of arthrogryposis multiplex congenita at term: congenital cytomegalovirus infection
- Mosaic trisomy 15 and prenatal genetic counselling: a case of Prader-Willi syndrome due to maternal uniparental disomy
- Prenatal detection and obstetric management of true umbilical cord knots using color Doppler and 4D ultrasonography: a report of two cases and literature review
- Three laparotomies later: extrinsic duodenal atresia from malrotation complicated by intrinsic duodenal and pyloric windsock webs
- Prenatal diagnosis of 17-hydroxylase/17,20-lyase deficiency (17OHD) in a case of 46,XY sex discordance and low maternal serum estriol
- Case Reports – Fetus
- A transient finding of fetal head entrapment caught in a uterine synechium or amniotic band
- Uncovering new physiology in bilateral renal agenesis following amnioinfusion
- Prenatal diagnosis of congenital mirror foot: case report and review
- A full-term infant with type II thanatophoric dysplasia
- Twin pregnancy in uteri with congenital anomalies: prenatal diagnosis by three- dimensional ultrasound
- Case Reports – Newborn
- Neonatal hemorrhagic shock as a consequence of ruptured velamentous vessels – a report of two cases
- Congenital multinodular goiter in a neonate presenting with airway obstruction

