Abstract
Amniotic fluid embolism (AFE) is an obstetrical catastrophe characterized by acute hypotension, hypoxia, and coagulopathy occurring during labor, cesarean section, post-delivery, or during amniocentesis. Thromboelastography (TEG) is a bedside test of global homeostasis and has seldom been used to study coagulation in AFE despite increasing popularity in other diseases. We report TEG usage as part of a treatment for patients with AFE.
Introduction
Amniotic fluid embolism (AFE) is an obstetrical catastrophe characterized by acute hypotension, hypoxia, and coagulopathy, which can occur during labor, cesarean section, post-delivery [2], or rarely, during amniocentesis [6]. We report the thromboelastogram findings of three women with AFE.
Thromboelastography (TEG) is a bedside test of global homeostasis and has seldom been used to study coagulation in AFE despite increasing popularity in other disease states. This, and the similar thromboelastometry (ROTEM) test, measure the viscoelastic properties of the blood clot. These properties are presumed to represent the coagulation profile of the patient. Although there are some differences between the tests, both TEG (Figure 1) and ROTEM assess the rotational changes of a system composed of a needle and cup. The blood is placed inside the cup and the needle is inserted into the blood. While the system rotates, the blood is allowed to coagulate. The coagulation process changes the rotational properties of the system and a computer draws a graph of the events. Despite the similarities between these two tests, there are some technical differences. In TEG, the cup is the rotating part, whereas in ROTEM, the needle rotates. Furthermore, the exact nomenclature is different between these exams. It should be noted, however, that although the information received is comparable, it cannot be transferred from one exam to the other [4, 9].

Normal thromboelastography tracing.
The normal ranges of its parameters are R (4–8 s), K (0–4 s), angle (47°–74°), and maximal amplitude (54–72 mm).
Case 1
A 40-year-old gravida 6, partum 5, with intact amniotic membrane had a sudden hemodynamic and respiratory collapse during post-term induction and augmentation of labor with oxytocin. Her cervical dilatation was 3 cm; she had no epidural and was monitored with continues external cardiotocography. The patient was rushed to the operating room for continued management and resuscitation, where a presumed perimortem cesarean section was performed. After the fetus was delivered, with continued resuscitation efforts, blood pressure was obtained. At this point, while continued administration of vasopressors and fluids, a transesophageal echocardiogram was performed. The test revealed elevated pulmonary pressures with acute cor pulmonale. No thrombus was detected in the main pulmonary trunk.
Following delivery, massive vaginal bleeding ensued, during which signs of disseminated intravascular coagulation were noticed by the surgical team. Coagulation tests taken after the initial administration of blood products (the patient received 8 units of packed blood cells, 21 units of thrombocytes, 10 units of fresh frozen plasma, and 30 units of cryoprecipitate) demonstrated a fibrinogen level of 170 mg/dL, international normalized ratio (INR) of 1.37, partial thromboplastin time (PTT) of 40.3 s, and platelet count of 103,000 μL. The TEG showed a low maximal amplitude (MA) of 42 mm, reflecting a decrease in clot strength (Figure 2).
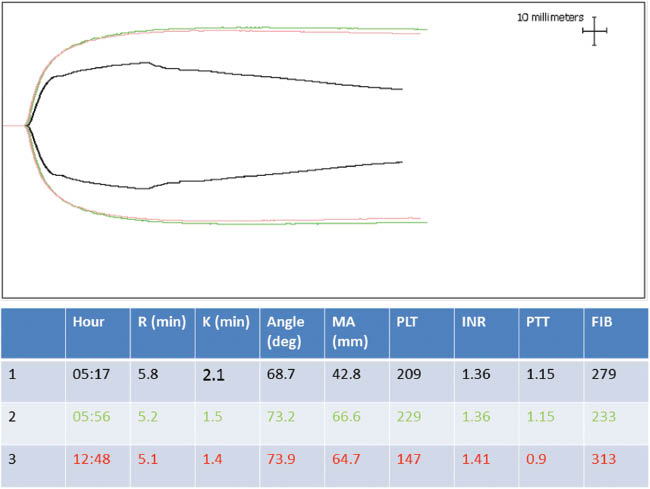
Thromboelastography (TEG) of the first case.
Trace 1 (black) was measured during administrating 8 units of plasma, 16 units of platelets, and 20 units of cryoprecipitate to the patient. It shows a decrease in the strength of the clot (low maximal amplitude). The second trace 2 (green) was recorded about 40 min later and it shows TEG parameters within normal limits. The third trace (red) was taken after the patients received 2 units of plasma, 5 units of platelets, and 10 units of cryoprecipitate. It is similar to the second trace.
Despite ongoing attempts to control the coagulopathy and blood loss, the bleeding continued. Subsequently, the patient underwent a hysterectomy resulting in the cessation of the hemorrhage. Pathological examination of the placenta revealed meconium staining. Postoperatively, she was admitted to the intensive care unit. She had received intravenous fluids, noradrenalin, dopamine, and inhaled nitric oxide as part of her treatment. Four days later, a repeated transthoracic echocardiography demonstrated normal pulmonary pressures and improved right ventricular function. The patient was subsequently extubated. She was discharged from the hospital several days later in good medical condition and with a healthy baby.
Case 2
Case 2 was a 35-year-old with hemodynamic and respiratory collapse with signs of angioedema at the end of an amniocentesis. The amniocentesis (30 mL) was performed due to polyhydramnios and esophageal atresia at a gestational age of 24±6 days. Her medical history included portal atresia and hypertension since birth, secondary to factor V Leiden homozygocity or umbilical vein cannulation as a premature infant. She had chronic thrombocytopenia with a platelet count of around 100,000 μL, with normal coagulation profile as recorded a year before this event and esophageal varices.
She received daily injections of enoxaparin that she withheld the day before the procedure. The amniocentesis was performed by a senior physician with a high volume of similar procedures. Towards the end of the procedure, the patient developed redness of her skin followed by facial swelling. Her blood pressure was unrecordable and her heart rate was 140 beats per minute. The presumed cause was thought to be a severe allergic reaction. After administration of adrenalin, subcutaneously and intravenously, and intravenous fluids, there was a systolic blood pressure of 70 mm Hg and oxygen saturation of 90%, while breathing from a reservoir mask. Following this initial period, blood tests were sent. Relevant results were a thrombocytopenia of 35,000 μL, an unrecordable INR, PTT, and fibrinogen level, furthermore, there was an increase in the hematocrit level from 30 to 55.
Her initial TEG did not show any coagulation activity (Figure 3). Her electrocardiography showed normal sinus rhythm and her chest X-ray showed a decrease in lung volume and bilateral pulmonary infiltrates. A bedside transthoracic echocardiogram demonstrated good left and right ventricular function. The patient received 20 units of cryoprecipitate and 2 units of fresh frozen plasma in addition to an adrenalin infusion and steroids. Her TEG improved with the appearance of coagulation and a decrease and normalization of the R time to <8 min.

Thromboelastography (TEG) of the second case.
The first trace (black) was taken before any blood product was administered to the patient. It shows that no coagulation was detected by the fact that it is a straight line and the international normalized ratio, partial thromboplastin time, and fibrinogen could not be measured. Trace number 2 (green) was taken about 3.5 h later, after administrating to the patient 2 units of plasma and 10 units of cryoprecipitate. Here there is a prolongation of R and K and decrease of the angle. These correspond to a delay in the initiation of the clot and of its propagation. Furthermore, the maximal amplitude severely decreased, aiming towards a weaker clot. The last trace (red) was taken after the patient received 10 units of cryoprecipitate. Although the R normalized, and there is improvement in the other parameters, there is still coagulopathy.
She later underwent feticide after severe neurological fetal impairment was noticed. However, in serial ultrasounds after the event, the amount of amniotic fluid was recorded to be normal (2 in the biophysical profile), and its AFI was 129 at an exam 2 days later. Due to a subsequent complaint of headache, computerized tomography of the brain was performed, which showed no pathology. She was discharged from the hospital in good health. Two years later, she delivered a normal healthy baby.
Case 3
A 39-year-old had a witnessed cardiorespiratory arrest at home in the 40th week of her 13th pregnancy. Advanced resuscitation was commenced at home by the paramedics ∼20 min after the collapse and she was transferred to the hospital with ongoing resuscitation. At the hospital, with the administration of pressors and inotropic agents, she had a recordable pulse and blood pressure. Due to fetal bradycardia, she was transferred to the operating room where a dead fetus was delivered by cesarean section. Later, at placental pathological exam, there was an evidence of meconium exposure. At this point, the patient became hypotensive and chest compressions were commenced. There was uterine atony and she was hemorrhaging massively. Coagulation tests showed that she was not clotting and the TEG was a straight line (Figure 4). Ten units of platelets and 10 units of cryoprecipitate were administered. A transesophageal echocardiogram demonstrated decreased right ventricular function and no thrombus in the pulmonary arteries. Despite all the measures taken to save her life, the patient was declared dead 2 h after being admitted to the hospital. No autopsies of the mother or the fetus had been done according to the request of the family.

Thromboelastography of the third case.
The black line demonstrates that no coagulopathy was detected. This trace is with correlation to the international normalized ratio, partial thromboplastin time, and fibrinogen that were undetectable. The trace was taken during the resuscitation efforts before blood products were administered.
Discussion
These three cases illustrate the TEG result in pregnant women with unexplained hemodynamic collapse, suspected to be AFE induced. The common denominator of the presented cases is severe coagulopathy that cannot be explained by the clinical context. The first and third cases demonstrate hemodynamic collapse with signs of right heart failure, without any evidence of thrombotic pulmonary emboli. In these two cases, there was hemorrhaging that came after a severe coagulation abnormality and initial stabilization. In this clinical setting, the diagnosis of AFE should be entertained as a diagnosis of exclusion.
Although there was no hemorrhaging in the second case, we think that AFE is a reasonable diagnosis. The patient underwent a procedure that has been described as one that can cause AFE [6]. She presented with hemodynamic collapse and dyspnea with signs of bilateral pulmonary infiltration on chest X-ray. Furthermore, she had signs of severe fluid sequestration and severe coagulopathy. It should be noted that this patient also had signs of angioedema and an allergic reaction. Indeed, this combination of symptoms and signs could be explained by a severe allergic/anaphylactic reaction. This, in turn, raises two important questions. First, what caused the allergic reaction? The patient had not been exposed to any new substances or medications. Among the treating team, there have been thoughts about latex or alcohexadine allergy; however, she had been exposed to these before, with no signs of adverse reaction. Second, fluid sequestration and coagulopathy have been described in anaphylaxis but they are not a common phenomenon (around 3% for coagulopathy) [8]. Therefore, we think that a diagnosis of AFE is reasonable in this setting.
A PubMed search with the words amniotic fluid embolism and thromboelastography or thromboelastograph found two case reports using ROTEM in AFE and two studies describing in vitro mixing of amniotic fluid with blood. Annecke et al. described thromboelastometry findings during treatment of a woman who suddenly collapsed after curettage for retained placental tissue [1]. The findings were no coagulation corresponding to heavy uterine bleeding. After treating her with tranexamic acid and infusion of blood products, there was clot formation with prolonged clotting time (correspond to R of the TEG), and low maximal clot strength (similar to MA of the TEG). Collins et al. presented a case of suspected amniotic fluid emboli and hemodynamic collapse after cesarean section [3]. The ROTEM results had shown hyperfibrinolysis and low fibrinogen. This woman was treated with antifibrinolitics and survived. Both these authors interpreted the coagulation results as being a result of increased fibrinolysis.
Harnett et al. added microliters of amniotic fluid to blood taken from pregnant women. R time was significantly decreased, platelet function was increased and there was no evidence of fibrinolysis [5]. Liu et al. demonstrated that when mixing amniotic fluid taken at midterm and term pregnancy with blood from healthy non-pregnant volunteers, coagulation accelerates, but there is no change in the MA or LY [7].
Annecke et al. interpreted no coagulation in the first thromboelastometry trace as a sign of extreme fibrinolysis and treated it with an antifibrinolytic agent and blood coagulation factors [1]. Collins et al. observed primary fibrinolysis and treated it with antifibrinolytics [3]. As opposed to Annecke and Collins, who interpreted their first trace as hyperfibrinolysis, we did not use antifibrinolytic agents, but rather plasma and cryoprecipitate, and our results were similar to Annecke’s and Collins’s second traces. Therefore, it seems that in our cases there was a strong component of coagulation factor deficiency rather than fibrinolysis.
The discrepancy in the results of the in vitro studies that show predominant hypercoagulation and the in vivo findings that show hypocoagulation may stem from the mix of microcirculatory clot formation and consumption coagulopathy. Another explanation of the findings could be a factor deficiency secondary to hemorrhage. We do not think that factor deficiency is the source of the hypocoagulopathy as it was present before the hemorrhaging, and was not observed in our second case.
We feel that point of care tests such as TEG or ROTEM have some advantages in these cases. Firstly, they help to narrow the differential diagnosis of the hemodynamic collapse from thrombus induced thromboembolism to that of AFE, ‘as in cases 1 and 3, where the results are not due to hypocoagulation, or severe allergic reaction (case 2), where coagulation abnormality is not so common. Furthermore, by its valuable point of care capabilities, the tests can guide the transfusion treatment required by these patients. In addition, they add some information about the pathophysiology of this deadly disease.
References
[1] Annecke T, Geisenberger T, Kürzl R, Penning R, Heindl B. Algorithm-based coagulation management of catastrophic amniotic fluid embolism. Blood Coagul Fibrinolysis. 2010;21:95–100.10.1097/MBC.0b013e328332cfe2Search in Google Scholar
[2] Clark SL, Hankins GD, Dudley DA, Dildy GA, Porter TF. Amniotic fluid embolism: analysis of the national registry. Am J Obstet Gynecol. 1995;172:1158–67.10.1016/0002-9378(95)91474-9Search in Google Scholar
[3] Collins NF, Bloor M, McDonnell NJ. Hyperfibrinolysis diagnosed by rotational thromboelastometry in a case of suspected amniotic fluid embolism. Int J Obstet Anesth. 2013;22:71–6.10.1016/j.ijoa.2012.09.008Search in Google Scholar
[4] da Luz LT, Nascimento B, Rizoli S. Thrombelastography (TEG®): practical considerations on its clinical use in trauma resuscitation. Scand J Trauma Resusc Emerg Med. 2013;16:21–9.10.1186/1757-7241-21-29Search in Google Scholar
[5] Harnett MJ, Hepner DL, Datta S, Kodali BS. Effect of amniotic fluid on coagulation and platelet function in pregnancy: an evaluation using thromboelastography. Anaesthesia. 2005;60:1068–72.10.1111/j.1365-2044.2005.04373.xSearch in Google Scholar
[6] Hasaart TH, Essed GG. Amniotic fluid embolism after transabdominal amniocentesis. Eur J Obstet Gynecol Reprod Biol. 1983;16:25–30.10.1016/0028-2243(83)90216-2Search in Google Scholar
[7] Liu EH, Shailaja S, Koh SC, Lee TL. An assessment of the effects on coagulation of midtrimester and final-trimester amniotic fluid on whole blood by thrombelastograph analysis. Anesth Analg. 2000;90:333–6.10.1213/00000539-200002000-00018Search in Google Scholar
[8] Pumphrey RS. Fatal anaphylaxis in the UK, 1992–2001. Novartis Found Symp. 2004;257:116–28.10.1002/0470861193.ch10Search in Google Scholar
[9] Sankarankutty A, Nascimento B, Teodoro da Luz L, Rizoli S. TEG® and ROTEM® in trauma: similar test but different results? World J Emerg Surg. 2012;7(Suppl 1):S3.10.1186/1749-7922-7-S1-S3Search in Google Scholar PubMed PubMed Central
-
The authors stated that there are no conflicts of interest regarding the publication of this article.
©2014 by Walter de Gruyter Berlin/Boston
Articles in the same Issue
- Frontmatter
- Case reports - Obstetrics
- Multiple embolizations of pulmonary arteriovenous malformations during pregnancy
- En caul vaginal delivery with vasa previa diagnosed intrapartum
- Successful vaginal packing in placenta previa
- Thromboelastography as a part of management of amniotic fluid embolism
- What enabled mother and twins to survive 18 minutes after maternal cardiopulmonary arrest?
- Placenta percreta after transcervical myomectomy
- Antenatal identification of factor VII Padua during a healthy pregnancy: implications for labor and delivery
- Case reports - Fetus
- Fetal posterior urethral valve mechanic perforation using an 18-gauge needle: a case-series
- Fetal ovarian cyst: 2- and 3-dimensional ultrasound as a new diagnostic method to rule out ovarian torsion
- Fetal chylous ascites may redevelop only after birth
- Triphasic umbilical artery waveform: association with severe fetal growth restriction, fetal demise, and extreme velamentous cord insertion
- Twin reversed arterial perfusion (TRAP) sequence managed at 11+6 weeks with radiofrequency ablation
- First trimester three-dimensional ultrasonographic diagnosis of diastrophic dysplasia: a case report and review of the literature
- Twin anemia-polycythemia sequence: the importance of an accurate diagnosis
- Prenatal diagnosis of fetal umbilical cord teratoma
- Recurrent fetal seizures diagnosed in the offspring of consanguineous parents
- Case reports - Newborn
- Spontaneous intestinal perforation and multiple thrombotic events in a neonate with thrombophilia
- Severe Bacillus cereus infection in a neonatal intensive care unit
- Non invasive nasal high frequency ventilation in the course of respiratory syncytial virus bronchiolitis
Articles in the same Issue
- Frontmatter
- Case reports - Obstetrics
- Multiple embolizations of pulmonary arteriovenous malformations during pregnancy
- En caul vaginal delivery with vasa previa diagnosed intrapartum
- Successful vaginal packing in placenta previa
- Thromboelastography as a part of management of amniotic fluid embolism
- What enabled mother and twins to survive 18 minutes after maternal cardiopulmonary arrest?
- Placenta percreta after transcervical myomectomy
- Antenatal identification of factor VII Padua during a healthy pregnancy: implications for labor and delivery
- Case reports - Fetus
- Fetal posterior urethral valve mechanic perforation using an 18-gauge needle: a case-series
- Fetal ovarian cyst: 2- and 3-dimensional ultrasound as a new diagnostic method to rule out ovarian torsion
- Fetal chylous ascites may redevelop only after birth
- Triphasic umbilical artery waveform: association with severe fetal growth restriction, fetal demise, and extreme velamentous cord insertion
- Twin reversed arterial perfusion (TRAP) sequence managed at 11+6 weeks with radiofrequency ablation
- First trimester three-dimensional ultrasonographic diagnosis of diastrophic dysplasia: a case report and review of the literature
- Twin anemia-polycythemia sequence: the importance of an accurate diagnosis
- Prenatal diagnosis of fetal umbilical cord teratoma
- Recurrent fetal seizures diagnosed in the offspring of consanguineous parents
- Case reports - Newborn
- Spontaneous intestinal perforation and multiple thrombotic events in a neonate with thrombophilia
- Severe Bacillus cereus infection in a neonatal intensive care unit
- Non invasive nasal high frequency ventilation in the course of respiratory syncytial virus bronchiolitis

